Early repolarisation pattern is defined electrocardiographically by a distinct J wave or J-point elevation that is either a notch or a slur of the terminal part of the QRS entirely above the baseline, with or without ST-segment elevation. The peak of the notch or slur (Jp) should be ≥0.1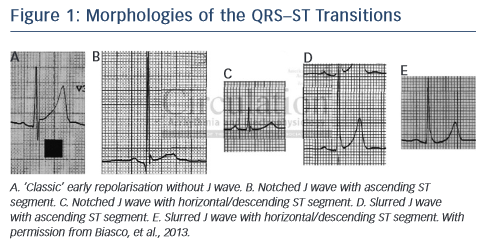 mV in two or more contiguous leads, excluding leads V1 to V2 (see Figure 1).1,2 Early repolarisation syndromes (ERS) refer to sudden cardiac death or documented VT/VF in individuals with an early repolarisation pattern. A prominent J wave has been long observed in cases of hypothermia hypercalcaemia and ischaemia.3 The term J-wave syndromes usually denotes inherited conditions such as ERS and the Brugada syndrome,4 which are due to mutations affecting calcium, potassium and sodium channels and may contribute to overlap syndromes.4,5
mV in two or more contiguous leads, excluding leads V1 to V2 (see Figure 1).1,2 Early repolarisation syndromes (ERS) refer to sudden cardiac death or documented VT/VF in individuals with an early repolarisation pattern. A prominent J wave has been long observed in cases of hypothermia hypercalcaemia and ischaemia.3 The term J-wave syndromes usually denotes inherited conditions such as ERS and the Brugada syndrome,4 which are due to mutations affecting calcium, potassium and sodium channels and may contribute to overlap syndromes.4,5
Genetics and Pathophysiology
The J-wave deflection occurring at the QRS–ST junction (also known as the Osborn wave) was first described in 1953 and is seen in many conditions such as acute ischaemia (especially in true posterior myocardial infarction), hypothermia, hypercalcaemia, brain injury, acidosis and early repolarisation syndromes. An increase in net repolarising current, due to either a decrease of inward Na+ or Ca2+ currents (INa, and ICa,L), or augmentation of outward currents, such as Ito, IK–ATP, and IK–ACh, lead to augmentation of the J wave or the appearance of ST-segment elevation that is more prominent during slow heart rates. Overlap with other syndromes may be seen. Mutations in the SCN10A gene may produce patterns of Brugada, early repolarisation and conduction disease,5 and a high prevalence of early repolarisation in short QT syndrome has also been reported.6 Physiological heterogeneity of electrical properties and transmural gradients in ion channel distribution in the endocardial, midmyocardial (M cells) and epicardial layers result in regional differences in electrophysiological properties. Ventricular epicardial (particularly RV) and M cells, but not endocardial action potentials, display a prominent phase 1 due to a large transient outward potassium current (Ito) giving rise to the typical spike and dome or notched configuration of the action potential and inscription of the J wave in the ECG. The degree of accentuation of action potential notch leading to loss of the dome depends on the magnitude of Ito. When Ito is prominent, as it is in the right ventricular epicardium, an outward shift of current causes phase 1 of the action potential to progress to more negative potentials at which the L-type calcium current (ICa,L) fails to activate, leading to all-or-none repolarisation and loss of the dome. Loss of the action potential dome usually is heterogeneous, resulting in marked abbreviation of the action potential at some sites but not at others. The dome then can propagate from regions where it is maintained to regions where it is lost, giving rise to local transmural reentry and closely coupled extrasystoles (phase 2 reentry). When the extrasystole occurs on the preceding T wave, it results in an R on T phenomenon that initiates polymorphic VT or VF.