How should Paced Patients who Report Syncope be Approached?
Syncope in the paced patient must be regarded as a serious symptom and be promptly investigated. The first consideration should be: was the correct diagnosis of the original syncope made? It is possible that syncope was reflex rather than conduction tissue disease. The second thought should be: are drugs playing a part? If the patient is hypertensive and on hypotensive treatment, this may be the cause of orthostatic hypotension or a rekindling of vasovagal syncope of youth. The third matter to consider is whether the pacing mode is correct. Patients with VVI pacing may have bouts of retrograde AV conduction that can precipitate syncope or, rarely, AAI mode has been selected for a patient with AVB. The fourth matter for thought is whether a tachyarrhythmia could be responsible for recurrence of syncope. In this instance, telemonitoring is extremely valuable for defining the arrhythmia. In such cases, assessment of left ventricular function by echocardiography may be helpful in showing deterioration of function that might be compatible with ventricular arrhythmias. Also, in the less likely possibility that atrial fibrillation is responsible for syncope, echocardiographic assessment of left atrial size is indicated.
Patients paced for AVB presenting syncope represent the most likely to have a pacing hardware fault as they are likely to be pacemaker dependent. First, it is necessary to make sure that the device is appropriate for the implanting indication and then consider the possibility of a technical fault. Always, it must be borne in mind that such faults may be difficult to identify in the clinic. In this instance, telemonitoring is much more effective.1
Early after implantation, the technical fault might be lead displacement or perforation or incomplete connection at the lead–pulse generator interface. Exit block may 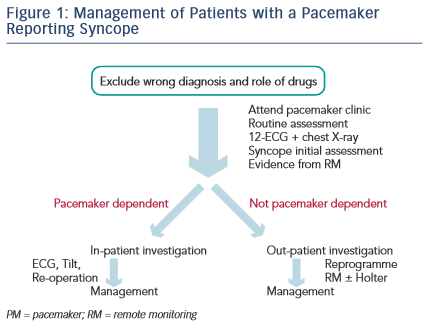 present early but also after the first month of implantation. The term ‘exit block’ implies that there is an excessive reaction by the endocardium at the site of the electrode, which has raised the stimulation threshold to a level above the output of the pacemaker. The pacemaker then fails to capture the heart. Some devices now measure the stimulation threshold and adjust output to address this problem. Later problems include lead insulation failure causing failure to capture heralded by low lead impedance, lead conductor fracture heralded by high lead impedance and possibly by oversensing. While these late problems are mostly lead related there could also be a pulse generator problem including normal or early battery depletion. Again, in all of these problems, telemonitoring is very important and must now be considered the standard of care.15
present early but also after the first month of implantation. The term ‘exit block’ implies that there is an excessive reaction by the endocardium at the site of the electrode, which has raised the stimulation threshold to a level above the output of the pacemaker. The pacemaker then fails to capture the heart. Some devices now measure the stimulation threshold and adjust output to address this problem. Later problems include lead insulation failure causing failure to capture heralded by low lead impedance, lead conductor fracture heralded by high lead impedance and possibly by oversensing. While these late problems are mostly lead related there could also be a pulse generator problem including normal or early battery depletion. Again, in all of these problems, telemonitoring is very important and must now be considered the standard of care.15
In patients with indications for pacing other than AVB, technical faults are also possible and must be excluded – telemonitoring is also ideal for this. After such a fault is considered very unlikely, a tilt test is advised to reveal a possible hypotensive tendency. If present, this may be the explanation for the patient’s problems but if absent hypotension could be considered unlikely. It should be borne in mind that a tilt test should no longer be taken as diagnostic but as a risk-of- syncope-recurrence stratification tool.11
The patient needs to be seen and, if known to be pacemaker dependent, perhaps directly admitted to hospital (see Figure 1). In clinic, the usual assessments must be made, also including deep respiration and movement of the pulse generator to attempt to expose evidence of lead damage. A 12-lead ECG must be taken, which is something often not done in the pacemaker clinic. The pattern of depolarisation may have changed from that after implant, implying lead displacement. A chest X-ray may be needed and may show evidence of lead displacement, lead damage or twiddler’s syndrome. The evidence from remote monitoring must be set against the data collected in the clinic. Is the pacing mode and programme correct? The initial assessment for syncope, as in the European Society of Cardiology Guidelines,16 should be undertaken as this may not have been done at implant. Last, the patient should be considered for admission to hospital – usually necessary for pacemaker-dependent patients, but unlikely to be necessary for patients not pacemaker dependent. For the non-dependent patient, remote monitoring should immediately be established if not already done. If remote monitoring is unavailable, prolonged Holter monitoring will often be required. Hospital admission is usually undertaken when a reoperation is needed rather than attempting therapy as a day case. It should be noted that diagnostic reoperation is now most unlikely to be needed because telemonitoring is so much more effective.
Patient management after diagnosis of the cause of syncope may be reoperation to correct the identified fault, lead repositioning, lead replacement, generator change or upgrading of the pacemaker system. In less serious problems, reprogramming may be sufficient. In reflex syncope cases, use of a rate-drop response type of pacemaker algorithm may help, especially making use of data from tilt testing to tune the program. A closed-loop pacemaker may be more effective than others in reflex syncope but no trial proof of this is currently available. For those who are tilt positive, attempting vasoconstrictor therapy with a drug such as midodrine may help. When it appears that sinus tachycardia is the trigger for syncope, antagonism of this by ivabradine or beta-blocker may help. These patients always need much reassurance because recurrence of pre-pacing symptoms does so much to undermine confidence.