Subjective Data
All participants in the analysis returned satisfactory training and symptom diaries, which were used in the subjective analysis. The most common cause of premature termination of training was back pain in the O65+ group (seven patients in the O65+ group [50 %], one patient in the O65− group [7 %] and one patient in the U65 group [8 %]). Time constraint was the reason for withdrawal in three patients in the U65 group (25 %) but none in either O65 group. Pre-syncopal symptoms were the reason for withdrawal in three patients in the O65+ group (15 %), two in the O65− group (14 %) and three in the U65 group (25 %). (Table 1). Comparison of the autonomic parameters pre- and post- training in those participants that experienced symptomatic benefit as opposed to those who did not revealed no significant differences.
Discussion
This prospective single-blind randomised trial is the first to assess HOT in an exclusively elderly population with VVS. Furthermore, with the exception of one study,19 all 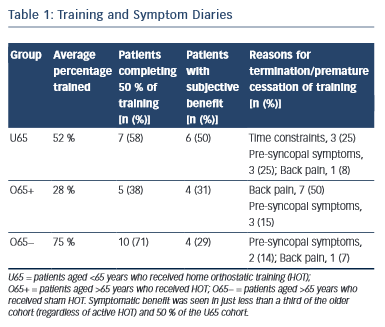 other randomised controlled trials20–21 examining the role of HOT have compared active orthostatic training to conventional therapy. The presence of the sham-training group in this study allows patient blinding to therapy and hence greatly strengthens the overall power. Unlike previous studies,19-20,22 no improvement in any autonomic cardiovascular reflex was observed in any of the study groups.
other randomised controlled trials20–21 examining the role of HOT have compared active orthostatic training to conventional therapy. The presence of the sham-training group in this study allows patient blinding to therapy and hence greatly strengthens the overall power. Unlike previous studies,19-20,22 no improvement in any autonomic cardiovascular reflex was observed in any of the study groups.
Early studies have assessed the changes in simple measures such as blood pressure, heart rate, time to first syncope and tilt-table result.17,21,23 These parameters have poor reproducibility24 and unless autonomic function is grossly altered, any subtle change will be lost in background noise. BRS and HRV spectral densities are being increasingly utilised as a sensitive research tool when looking at autonomic responses. The high sensitivity is in part because of the exponential changes in these values as opposed to linear changes in the traditionally-measured parameters. HRV spectral density plots show two regions of interest when considering the activity of the autonomic system. LF-HRV changes during respiration and is thought to reflect sympathetic activity, whilst HF-HRV is thought to represent parasympathetic activity.25
Tilt-table testing in patients with VVS has shown a reduced BRS at rest and an exaggerated drop in BRS during HUTT.26 Changes in HRV have been less consistent in patients with VVS with the exception of LF-HRV response, which is diminished.27
The aim of orthostatic training is to modify these autonomic responses in patients to induce a normalised response to orthostatic stress and therefore preventing the symptoms of VVS.
The expected benefit in our actively-trained elderly group was not observed. One reason that might account for this is that VVS has been shown to be bi-modally distributed across the population, with peaks between20–29 years and an older cohort aged >70 years.17 This suggests that the VVS mechanism in these two groups may have some important differences that may explain the lack of efficacy of HOT seen in this trial. It is well-documented that autonomic responses are blunted in an elderly population.28 This depression of the autonomic response may account for the observed HUTT differences, with younger patients having a more pronounced and rapid-onset bradycardia with hypotension (classical response), whilst the elderly population tends to have a slower, asymptomatic onset of hypotension with a less pronounced bradycardia (dysautonomic response),29 as observed in our study cohorts. Younger patients also exhibit the classical warning signs of an exaggerated autonomic response of pallor, sweatiness, abdominal discomfort and light-headedness whilst the older population do not.4 It is therefore conceivable that orthostatic training in an elderly population may not enhance an age-related degenerated autonomic system whereas in a younger group, HOT may be able to ‘retrain’ an exaggerated or inappropriate autonomic response.
However our results show little effect of HOT in the younger control patients. The explanation for this lack of response is not clear. Previous studies have shown that the mechanism of VVS may begin to change from a predominately exaggerated autonomic response to a depressed autonomic response in patients in their forties.19 Almost two thirds of the younger cohort were aged >50 years, which may have resulted in a HOT response similar to that in the O65 actively-trained cohort. All previous studies have shown benefit from HOT in younger patients (mean ages 16.0 years,17 45.0 years,19 31.0 years22 and 19.4 years.21)
Most participants had no symptoms for the duration of the study. It has been shown that the autonomic improvements provoked by orthostatic training can be observed within 1 week of training initiation19 and that HUTT maybe rendered negative within 24 hours of in-hospital training.22 It is possible that these autonomic benefits may be lost at a similar rate on cessation of training. With a low symptom burden the participants training regime may not have been adhered to as strictly as reported.
Back pain was the most commonly reported cause of lack of HOT compliance. This was worse in the elderly cohort. In the younger group, lack of time and pre-syncopal symptoms were the most common causes of failed compliance. Overall compliance was comparable with previous studies demonstrating autonomic improvements from HOT.19
Study limitations
Participant record of compliance could not be verified beyond self-reporting, and records may be an overestimation of actual time trained. Despite this, even participants who reported great symptomatic benefit from the training showed no change in objectively assessed autonomic measures.