Heart Failure – A Major Global Health Problem
Cardiovascular diseases (CVDs) remain the leading cause of morbidity and mortality in developed countries and its burden is progressively increasing.1–4 Coronary artery disease (CAD) and other conditions, such as hypertensive heart disease or diabetes mellitus, are rated among the foremost reasons for morbi-mortality worldwide.1–4 In this context, heart failure (HF) has emerged as an extremely important condition that appears to be reaching epidemic proportions. The reported prevalence and incidence of HF varies depending on the studies considered, the definitions used, subjects included in studies and quality of data recorded.5,6 An overall prevalence of 1–2 % has generally been reported in western countries,5–7 and this is considerably high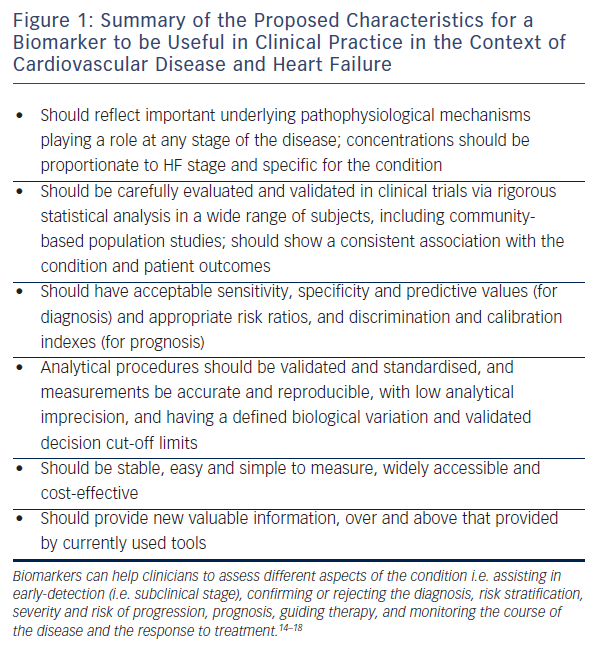
Biomarkers in Heart Failure
HF is primarily diagnosed in the presence of symptoms and signs that, in many cases, are non-specific.7,12 Symptoms of HF result from an impairment in the normal heart function as a consequence of structural or functional disorders affecting ventricular filling and/or blood ejection.7,12 Recently, biomarkers such as brain natriuretic peptide (BNP) or amino-terminal pro-brain natriuretic peptide (NT-proBNP) have emerged, which appear to represent an important tool for diagnosis, risk stratification and prognosis.7,12 A biomarker has been defined as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention”.13 Although this definition is wide and can include any measured parameter, the term ‘biomarker’ is more commonly used in relation to biological substances that are detected in body fluids. Figure 1 summarises the characteristics that make a biomarker useful in clinical practice in the context of CVD and HF.14–18