Diagnosis
Although there is increasing awareness among clinicians regarding pulmonary hypertension, much more work needs to be carried out to promote earlier and accurate diagnosis. The clinical features are often non-descript and include fatigue, malaise, chest pain, palpitations, pre-syncope or syncope or haemoptysis. Additionally, the diagnosis may not be considered in patients with co-existing cardiac or pulmonary disease and yet underlying pulmonary hypertension may be the reason for the apparent failure to respond to conventional treatment of their primary disease. Furthermore, it is essential that pulmonary hypertension is carefully assessed and optimised where appropriate if patients are required to undergo intervention (e.g surgery) or should they become pregnant. In addition to history and clinical examination the following investigations are routinely performed to assess patients with suspected pulmonary hypertension;
This investigation is considered gold standard for diagnosing patients with pulmonary hypertension and provides information regarding right arterial pressure, pulmonary arterial pressure, right ventricular pressure, cardiac output and mixed venous (pulmonary arterial) oxygen saturation and left atrial filling pressure (the pulmonary capillary wedge pressure). The pulmonary vascular resistance (PVR) is derived from the formula: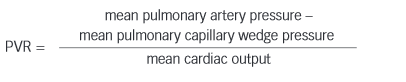
The PVR can be indexed (PVRi) and the systemic vascular resistance can also be calculated and indexed (SVRi).
Other tests that may be performed include exercise test, magnetic resonance imaging (MRI), overnight oximetry and, occasionally, pulmonary angiogram.
Disease Progression
At onset there may be few symptoms, but as the disease progresses the PVR rises and the cardiac output falls. Common symptoms include dyspnoea on exertion or at rest, chest pain (due to right ventricular angina), palpitations and pre-syncope or syncope. Ultimately the signs and symptoms of right heart failure develop and death occurs. A median survival of 2.8 years has been reported for untreated patients in New York Heart Association (NYHA) class III or IV. Sudden acute elevations in PVR can occur (known as pulmonary hypertensive crises) leading to an acute reduction in left heart filling and profound systemic hypotension and can sometimes be fatal. This can occur during general anaesthetic induction and is one of the reasons why patients with PAH need careful preoperative evaluation prior to surgical intervention.