Treatment Guidelines
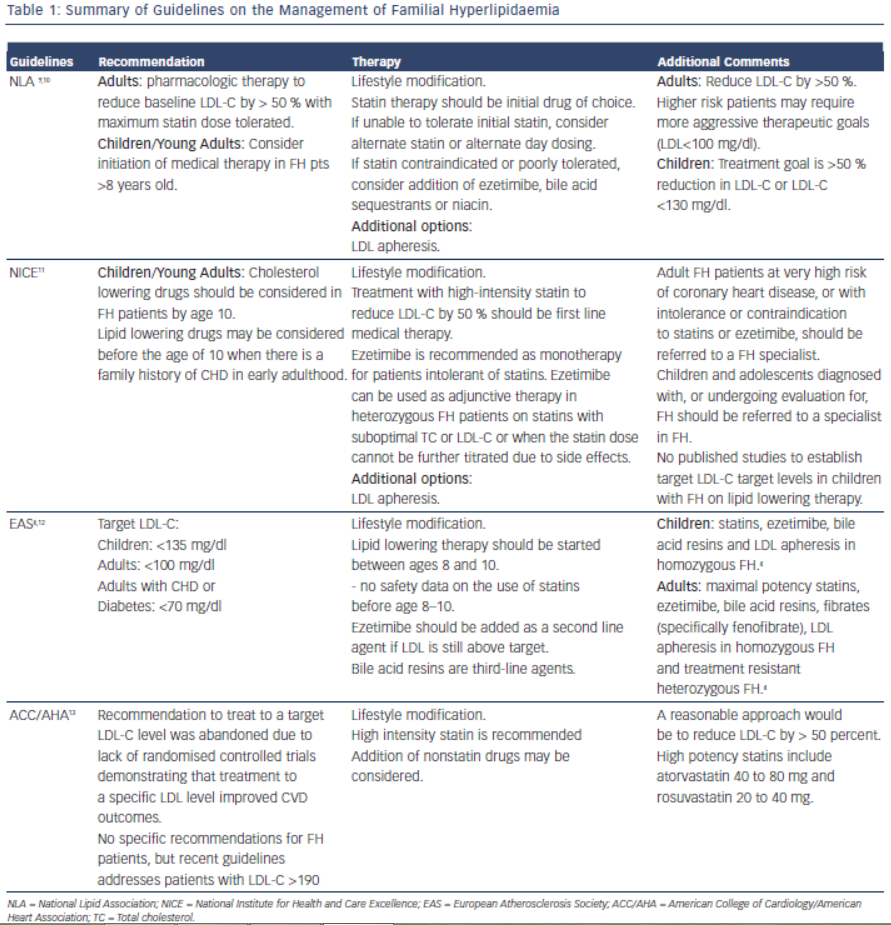
Early detection and treatment of FH is recommended to reduce risk of cardiovascular events. The goal of treatment is to reduce LDL-C by 50 % from baseline levels.9 This was based on two trials which showed reduction in CIMT (Carotid Intimal Medial Thickness) in patients who achieved > 50 % reduction of LDL-C on statin therapy.10,11 Lifestyle modification, lipid-lowering therapy, LDL apheresis and in rare cases, liver transplant are the cornerstones of LDL-C lowering in patients with FH. Table 1 summarises the current guidelines for the treatment of FH.
It is important for the clinician to be aware of the various treatment options for FH, as combination therapy will likely be required to achieve goal reductions in LDL-C. Investigators have reported as many as 77 % of patients with an FH diagnosis and on cholesterol medication do not achieve goal LDL-C levels within two years of diagnosis.12 The most common reason cited (32 %) for inadequate control of the patients’ cholesterol levels was “acceptance” of a suboptimal LDL-C level by a treating physician.13 Other causes of inadequate control include improper dosing of medications and late age of diagnosis.14
Lifestyle Modifications
Lifestyle modification is the foundation in the treatment of FH. Primordial prevention which includes counselling for smoking, avoidance of diabetes and regular physical activity is an integral component for treatment in this population.1 Dietary recommendations from the National Lipid Association and International FH Foundation include are outlined in Table 2.15 These groups’ recommendations also emphasise limiting alcohol intake (one drink daily for women, 1-2 drinks daily for men) and tobacco cessation.16 Referral to appropriately qualified nutritionists and dieticians is also recommended.2 Daily physical activity is encouraged, and achieving an optimal weight for overweight patients should be stressed. For every 10 kg of weight lost, there is an 8 mg/dl reduction of LDL-C.17,18 While lifestyle modification is the first step in the treatment of FH patients, this strategy alone will be insufficient as the sole treatment to achieve LDL-C goal. Lifestyle modification will at most reduce LDL-C concentration by 10–15 %19 and most patients will require further pharmacological therapy.
Pharmacologic Treatment
Patients with LDL >190 mg/dl are identified within the new ACC/ AHA 2013 Blood Cholesterol Guidelines as requiring pharmacologic intervention.20 The required treatment regimen and the individual’s response to this treatment varies according to the genetic and phenotypic heterogeneity of FH, with autosomal recessive hypercholesterolaemia responding more robustly to treatment.1
Statins
Statins inhibit hydroxyl-methylglutaryl coenzyme A reductase (HMGCoAR), a key enzyme in the synthesis of cholesterol in the liver, ultimately decreasing LDL production. Statins also lead to up-regulation of LDL receptors; however this effect is limited due to enhanced compensatory degradation of such receptors. In patients with HoFH, the effectiveness of statins is attenuated given its mechanism of action involves up-regulation of liver LDL receptors. This is the case also for ezetimibe and bile acid sequestrants.21
Statins are first line pharmacologic therapy agents in the treatment of FH; they reduce cardiovascular mortality even in receptor-negative patients.22
 Current guidelines recommend maximal statin therapy to reduce LDL-C levels by at least 50 % from baseline.20,23–25 Therapy should be started with a high potency statin at the greatest tolerated dose. Plasma levels of hepatic transaminases, creatine kinase (CK), glucose and creatinine should be measured before starting drug therapy.
Current guidelines recommend maximal statin therapy to reduce LDL-C levels by at least 50 % from baseline.20,23–25 Therapy should be started with a high potency statin at the greatest tolerated dose. Plasma levels of hepatic transaminases, creatine kinase (CK), glucose and creatinine should be measured before starting drug therapy.
Despite aggressive statin therapy, in the majority of patients with FH, even the highest doses of the most potent statins do not yield more than a 50 % LDL-C reduction. In these patients a combination of lipidmodifying agents enhances efficacy.3,21,22,26–28 Most often, the cholesterol absorption inhibitor Ezetimibe is chosen as second line therapy.3