However, macrovascular complications gradually emerge long before the actual diagnosis of DM occurs, due to impaired glucose tolerance characterised by long-standing insulin resistance, compensatory hyperinsulinaemia and varying degrees of elevated plasma glucose, which lead in the end to the onset of DM.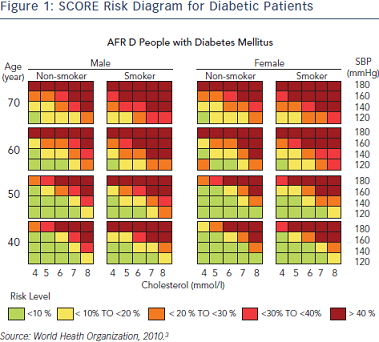 This process is identified by the development of an atherosclerotic plaque, which in the presence of enhanced inflammatory content becomes unstable and prone to rupture. Atheroma from patients with DM has more lipid, inflammatory changes and thrombus than a normal subject.1 By contrast, microvascular complications slowly begin to unfold only after the onset of clinical diabetes. Two important trials, Diabetes Control and Complication Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS), have demonstrated the continuous relationship between the increase of HbA1c and microvascular complications, without an apparent threshold.5 Conversely, a decrease by 2 % in HbA1c significantly lowers the risk of developing nephropathy and retinopathy in DM type 1.6
This process is identified by the development of an atherosclerotic plaque, which in the presence of enhanced inflammatory content becomes unstable and prone to rupture. Atheroma from patients with DM has more lipid, inflammatory changes and thrombus than a normal subject.1 By contrast, microvascular complications slowly begin to unfold only after the onset of clinical diabetes. Two important trials, Diabetes Control and Complication Trial (DCCT) and United Kingdom Prospective Diabetes Study (UKPDS), have demonstrated the continuous relationship between the increase of HbA1c and microvascular complications, without an apparent threshold.5 Conversely, a decrease by 2 % in HbA1c significantly lowers the risk of developing nephropathy and retinopathy in DM type 1.6
Assessing cardiovascular risk in patients with DM can be achieved through various methods, one of the most popular being the Systematic Coronary Risk Evaluation (SCORE) risk diagrams. According to these, DM or chronic kidney disease, or very elevated cholesterol or blood pressure places the patient at a high risk (5–10 %) of developing a fatal cardiovascular event in the next ten years (see Figure 1).
On the other hand, assessing the risk of type 2 DM can be conducted using the Finnish Diabetes Risk Score (FINDRISC) questionnaire, which addresses the risk of developing type 2 DM in the next ten years, by dividing it in low, moderate, high and very high risk.
CAD accounts for over 60 % mortality in people with DM, more than twice the non-diabetic population, while impaired glucose metabolism, comprising of impaired fasting glycaemia and impaired glucose tolerance, is also linked to CAD – since moderately elevated glucose levels below the threshold for DM also represent an increased risk.7 Moreover, established DM is associated with impaired prognosis after myocardial infarction.8 The Euro Heart Survey programme carried out a study on diabetes and the heart, trying to assess the prevalence of DM and impaired glucose regulation in adult patients with CAD, and to compare diagnostic and therapeutic tools suitable for these patients.9 In their 4,961 cohort of people from 110 European countries admitted with CAD, only 29 % with acute CAD and 34 % with stable CAD were normoglycaemic, thereby concluding that it was unusual to have normal glucose tolerance in patients with CAD.9 The results from the Euro Heart Survey showed that out of the population classified as normoglycaemic by the WHO criteria of 1999 (fasting plasma glucose <6.1 mmol/L), when performed an oral glucose tolerance test, 27 % of these patients proved to have impaired glucose tolerance and 8 % diabetes. Five percent of the group with impaired fasting glucose proved to have actual diabetes. Judging by the American Diabetes Association (ADA) criteria of 2003 (fasting plasma glucose <5.6 mmol/L), 21 % of the normoglycaemic patients were discovered to have impaired glucose tolerance, while 5 % diabetes.9 However, abnormal glucose tolerance seems to be quite common in the general population, as a study on the Australian population aged 65 discovered similar results, 8 % having undiagnosed diabetes and 25 % impaired glucose metabolism.10 While this conclusion appears to be true, it also suggests that it is more common in people with CAD and that an oral glucose tolerance test should be performed on a routine basis for such patients, as fasting glycaemia proves to be insufficient.9
An international expert committee issued a report in 2009 on the role of HbA1c in diagnosing diabetes and concluded that HbA1c between 5.7 % and 6.5 % places the patient at high-risk for developing diabetes, while values over 6.5 % signify undiagnosed diabetes.11
UKPDS, a landmark study with a major impact on clinical care, showed that in newly diagnosed patients with type 2 DM, intensive glucoselowering therapy reduced the risk for clinically important diabeticrelated endpoints. Although mortality and cardiovascular events were not reduced in the main trial, important benefits emerged during a 10-year post-trial monitoring, including a 24 % reduction in microvascular disease, a 15 % reduction in myocardial infarction and lower mortality.13 The most controversial of recent trials is the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, which tested the hypothesis that when compared with conventional therapy, normalising glucose levels (target HbA1c 6.0 %) would reduce incident cardiovascular death or events in high-risk patients with type 2 DM.14 After 3.5 years, the trial was stopped prematurely because of a 22 % higher mortality in the intensive therapy group.