Bifurcation Disease—Classification and Percutaneous Therapeutic Options
Within the spectrum of complex coronary lesions approachable by PCI, bifurcation disease merits special 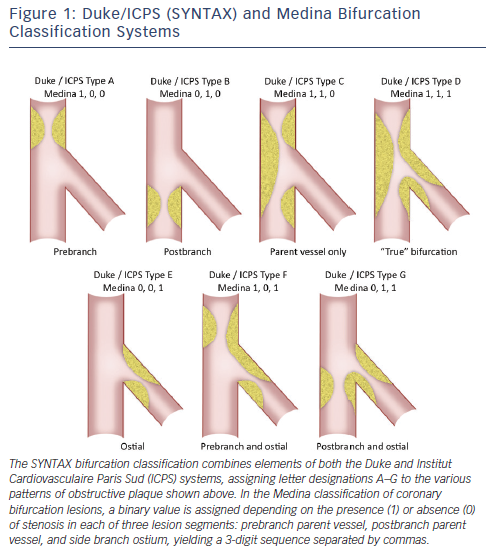 consideration as it is encountered frequently, accounting for 15-25 % of PCIs in some series, and has been associated with higher-than-average technical complexity and lower success rates.7,17,18 Optimal percutaneous treatment of bifurcation disease is guided by an extensive body of bench and clinical investigation with available data bearing out the potential consequences of inappropriate treatment, such as restenosis and/ or thrombosis of one or both vessels involved. Multiple bifurcation classification systems have been developed with the common goal of clarifying optimal interventional strategy and predicting complication risk.17–20 All schemas quantify the extent and location of plaque burden with some also incorporating the angle between parent and daughter vessel. The SYNTAX bifurcation classification, modified from the wellknown Duke and Institut Cardiovasculaire Paris Sud (ICPS) criteria, along with the Medina classification, representing a contemporary, simplified system, are shown in Figure 1.13,20,21 Side branch angulation is missing from both of these classification systems, although it is now well-recognized as an additional metric with important prognostic value.21 Whichever the system applied, ‘true’ bifurcation disease is characterized by obstructive disease in the parent vessel, pre- and post-side branch, as well as obstructive disease within the ostium of the side branch.
consideration as it is encountered frequently, accounting for 15-25 % of PCIs in some series, and has been associated with higher-than-average technical complexity and lower success rates.7,17,18 Optimal percutaneous treatment of bifurcation disease is guided by an extensive body of bench and clinical investigation with available data bearing out the potential consequences of inappropriate treatment, such as restenosis and/ or thrombosis of one or both vessels involved. Multiple bifurcation classification systems have been developed with the common goal of clarifying optimal interventional strategy and predicting complication risk.17–20 All schemas quantify the extent and location of plaque burden with some also incorporating the angle between parent and daughter vessel. The SYNTAX bifurcation classification, modified from the wellknown Duke and Institut Cardiovasculaire Paris Sud (ICPS) criteria, along with the Medina classification, representing a contemporary, simplified system, are shown in Figure 1.13,20,21 Side branch angulation is missing from both of these classification systems, although it is now well-recognized as an additional metric with important prognostic value.21 Whichever the system applied, ‘true’ bifurcation disease is characterized by obstructive disease in the parent vessel, pre- and post-side branch, as well as obstructive disease within the ostium of the side branch.
Even more numerous than bifurcation classification systems are the technical approaches described to date, varying widely in terms of the number of stents mandatorily used, completeness of coverage of the side branch ostium, and procedural complexity. A consensus classification of families of bifurcation techniques was  proposed by the European Bifurcation Club (EBC) some years ago.21,22 This system, referred to as the MADS classification, is an acronym with each letter corresponding to a different choice for first vessel/segment addressed and approach to initial stent deployment. ‘M’ stands for Main proximal vessel first, ‘A’ for main Across side branch first, ‘D’ for Distal first, and ‘S’ for Side branch first. Various bifurcation techniques, including those double-stent techniques detailed in Figure 2 along with several others, are categorized under each lettered group and further broken out by the use of one, two, or three stents. Two-stent techniques that do not insure complete side branch coverage include the variations on the T-stent technique (see Figure 2) including classical and reverse T-stenting. More advanced techniques that allow for complete side branch coverage include variations on crush stenting, culotte stenting, and classical or modified simultaneous kissing stent (SKS) techniques.17,20,22
proposed by the European Bifurcation Club (EBC) some years ago.21,22 This system, referred to as the MADS classification, is an acronym with each letter corresponding to a different choice for first vessel/segment addressed and approach to initial stent deployment. ‘M’ stands for Main proximal vessel first, ‘A’ for main Across side branch first, ‘D’ for Distal first, and ‘S’ for Side branch first. Various bifurcation techniques, including those double-stent techniques detailed in Figure 2 along with several others, are categorized under each lettered group and further broken out by the use of one, two, or three stents. Two-stent techniques that do not insure complete side branch coverage include the variations on the T-stent technique (see Figure 2) including classical and reverse T-stenting. More advanced techniques that allow for complete side branch coverage include variations on crush stenting, culotte stenting, and classical or modified simultaneous kissing stent (SKS) techniques.17,20,22
The results of numerous published clinical trials and registries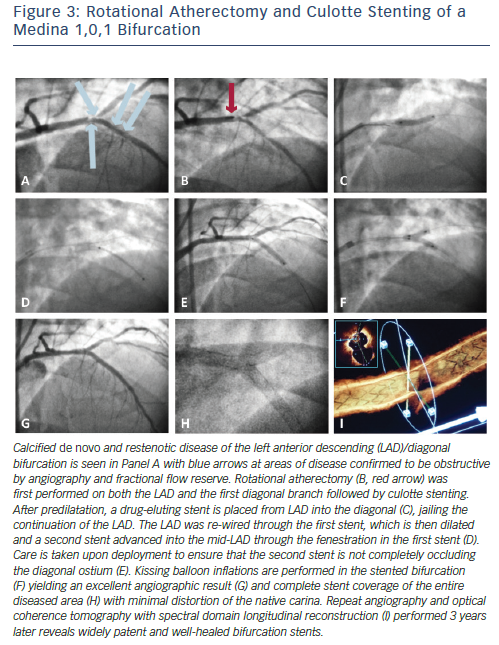 of bifurcation technique have been evaluated in the context of several meta-analyses.23–31 These systematic reviews have found with great consistency that in the current era of DES, a simple, single-stent strategy using provisional side branch stenting, when feasible, is superior to complex (double stent) strategies with respect to rates of myocardial infarction and stent thrombosis.23–31 If a satisfactory angiographic result is obtained with parent vessel stenting ± side branch ballooning, forgoing side branch stenting is appropriate based on the available data and, moreover, will save on procedural time and cost, radiation exposure, and contrast usage.17,20–22 As fractional flow reserve (FFR) was demonstrated to be an important discriminatory tool for guiding the performance of single- or multivessel PCI in the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME-2) study, so too has the value of FFR been demonstrated in assessing the functional significance of jailed side branch stenoses.32 Ahn et al. studied 230 jailed side branch stenoses in bifurcation lesions where main vessel stenting was performed and found that only 17.8 % of jailed side branch lesions were associated with functional significance (FFR <0.80).33 Moreover, visual discrimination of ‘significant’ side branch stenoses by angiography alone was limited at best.
of bifurcation technique have been evaluated in the context of several meta-analyses.23–31 These systematic reviews have found with great consistency that in the current era of DES, a simple, single-stent strategy using provisional side branch stenting, when feasible, is superior to complex (double stent) strategies with respect to rates of myocardial infarction and stent thrombosis.23–31 If a satisfactory angiographic result is obtained with parent vessel stenting ± side branch ballooning, forgoing side branch stenting is appropriate based on the available data and, moreover, will save on procedural time and cost, radiation exposure, and contrast usage.17,20–22 As fractional flow reserve (FFR) was demonstrated to be an important discriminatory tool for guiding the performance of single- or multivessel PCI in the Fractional Flow Reserve versus Angiography for Multivessel Evaluation 2 (FAME-2) study, so too has the value of FFR been demonstrated in assessing the functional significance of jailed side branch stenoses.32 Ahn et al. studied 230 jailed side branch stenoses in bifurcation lesions where main vessel stenting was performed and found that only 17.8 % of jailed side branch lesions were associated with functional significance (FFR <0.80).33 Moreover, visual discrimination of ‘significant’ side branch stenoses by angiography alone was limited at best.
However, specific situations exist where one may wish to commit early to a complex bifurcation strategy. Intermediate to large side branches (>2.5 mm diameter), particularly those that are comparably sized as the parent vessel, side branches evidencing contiguous obstructive disease extending away from the ostium, side branch territories with demonstrable ischemia, or significant/flow-limiting dissection may merit consideration of a more complex bifurcation strategy with deliberate stenting of the side branch. Figure 3 depicts step-wise detail of a culotte stenting procedure in which calcified de novo and restenotic disease in the bifurcation of an LAD and large diagonal branch warranted a complex, multistent approach following debulking with rotational atherectomy. In planning percutaneous therapy for complex bifurcation disease, careful pre-procedure consideration of the coronary anatomy, aforementioned criteria, and various technical strategies, is therefore warranted.17,20–22