 First Data on Bioresorbable Vascular Scaffolds Used for Treating Bifurcation Lesions
First Data on Bioresorbable Vascular Scaffolds Used for Treating Bifurcation Lesions
BVS implantation was initially only recommended for simple lesions, avoiding side branch anatomy. There was the concern that after rewiring the side branch, ostial side branch dilatation might damage the BVS. Indeed, in the instructions for use, the manufacturer, Abbott Vascular, warns that lesions with 2 mm side branches should be avoided. At the same time, preliminary data indicate that 1.5 mm and 2.0 mm balloons taken to nominal pressure will not cause mechanical disruption of the BVS. However, a 2.5 mm balloon might cause disruption of the longitudinal crosslinks, but without impacting radial strength.15 Others have suggested that the cells of a 2.5 mm BVS can be crossed with a second wire and be dilated with a non-compliant balloon up to a diameter of 3.0 mm without strut fracture.16
A clinical case report implies it may indeed be possible to carefully dilate side branches without severe 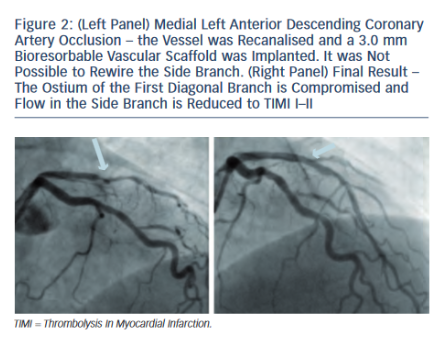 structural damage to the BVS in the main vessel.17 Gogas et al. performed a bailout procedure after implantation of a 3.0 mm BVS in the left anterior descending coronary artery (LAD). While the result in the LAD itself was entirely satisfactory, the second diagonal branch, covered by the BVS, showed subtotal occlusion and Thrombolysis In Myocardial Infarction (TIMI) flow grade 1.17 Although the side branch diameter was only 1.7 mm, the patient experienced chest pain, and the operators decided to re-cross the BVS cells. The ostium of the side branch was dilated with a 1.5 mm compliant balloon, restoring normal flow. The immediate angiography result was very good, and an additional analysis by using optical coherence tomography (OCT) confirmed adequate strut apposition and lack of fractures.17
structural damage to the BVS in the main vessel.17 Gogas et al. performed a bailout procedure after implantation of a 3.0 mm BVS in the left anterior descending coronary artery (LAD). While the result in the LAD itself was entirely satisfactory, the second diagonal branch, covered by the BVS, showed subtotal occlusion and Thrombolysis In Myocardial Infarction (TIMI) flow grade 1.17 Although the side branch diameter was only 1.7 mm, the patient experienced chest pain, and the operators decided to re-cross the BVS cells. The ostium of the side branch was dilated with a 1.5 mm compliant balloon, restoring normal flow. The immediate angiography result was very good, and an additional analysis by using optical coherence tomography (OCT) confirmed adequate strut apposition and lack of fractures.17
A complex bifurcation lesion was treated by Naganuma et al.18 They recanalised a chronic total occlusion of the left circumflex coronary artery (LCx), placing a wire in the LCx itself and another one in the first obtuse marginal branch (OM1). First, a BVS was implanted in the OM1-ostium. Subsequently, two BVS were implanted in the LCx, covering the ostium of the OM1. Given a very convincing angiographic appearance, the OM1 was not rewired. Post-procedural intravascular ultrasound analysis demonstrated well-apposed BVS struts in the LCx. The OM1 was not separately interrogated.18
What to Expect
It is to be expected that many reports, including series of patients, will follow these preliminary case reports. At the annual European and American  interventional meetings, several case reports have been presented, reaffirming the feasibility of treating bifurcation lesions by using BVS. Compared with modern DES, rewiring the side branch is more difficult mainly because of the greater BVS strut thickness. Indeed, it can be even tricky to advance a second guidewire through the BVS within the main vessel, all the more a second BVS.
interventional meetings, several case reports have been presented, reaffirming the feasibility of treating bifurcation lesions by using BVS. Compared with modern DES, rewiring the side branch is more difficult mainly because of the greater BVS strut thickness. Indeed, it can be even tricky to advance a second guidewire through the BVS within the main vessel, all the more a second BVS.
This may indicate that the success rate regarding side branch interventions might be inferior using BVS compared with modern DES. However, once the side branch has been rewired, crossing the BVS cells with a balloon appears to be rather simple. However, it is currently unclear up to what size balloons can be inflated without disrupting the cells of the BVS or impacting its radial strength. Certainly, there is a risk that kissing balloon inflation will damage the main vessel BVS, and it should probably be avoided. If deemed absolutely necessary, moderate balloon sizing and inflation pressures should be chosen. Preferentially, if yearning to protect the BVS from malapposition, sequential balloon inflation should be performed first in the side branch and then in the main vessel (see Figures 1-3).
 An important question relates to the necessity of performing side branch dilatation. Will this be needed in a sizeable number of BVS interventions? A recent analysis from the ABSORB-EXTEND (A Continuation in the Clinical Evaluation of the ABSORB Bioresorbable Vascular Scaffold [BVS] System in the Treatment of Subjects With de Novo Native Coronary Artery Lesions) single-arm trial compared the rate of side branch occlusion in 435 patients treated by using BVS implantation to a historic control group of 237 patients with DES (Abbott XIENCE V) implantation in the SPIRIT first and SPIRIT II (A Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System in the Treatment of Patients With de Novo Native Coronary Artery Lesions) trials.19
An important question relates to the necessity of performing side branch dilatation. Will this be needed in a sizeable number of BVS interventions? A recent analysis from the ABSORB-EXTEND (A Continuation in the Clinical Evaluation of the ABSORB Bioresorbable Vascular Scaffold [BVS] System in the Treatment of Subjects With de Novo Native Coronary Artery Lesions) single-arm trial compared the rate of side branch occlusion in 435 patients treated by using BVS implantation to a historic control group of 237 patients with DES (Abbott XIENCE V) implantation in the SPIRIT first and SPIRIT II (A Clinical Evaluation of the XIENCE V Everolimus Eluting Coronary Stent System in the Treatment of Patients With de Novo Native Coronary Artery Lesions) trials.19
The angiographic analysis documented a mean of 2.8 side branches in the BVS group and 2.9 in the DES group. Side branch occlusion occurred in 6.0 % in the BVS group and in 4.1 % in the DES group (p=0.09). The incidence of side branch occlusion appeared to depend on side branch vessel diameter. Whereas occlusion was clearly more frequent in small side branches with an angiographic diameter 0.5 mm, no statistic difference was observed in larger side branches (see Figure 4).19 These data suggest that with regard to important side branches, the occlusion rates are similar between BVS and modern DES, and the necessity to perform a bifurcation procedure should be comparable.