Issues Related with Stent Implantation in the Main Vessel
After wiring both branches and pre-dilation, when appropriate, the stent is deployed in the MV across the SB. As a first point, it must be emphasised that with 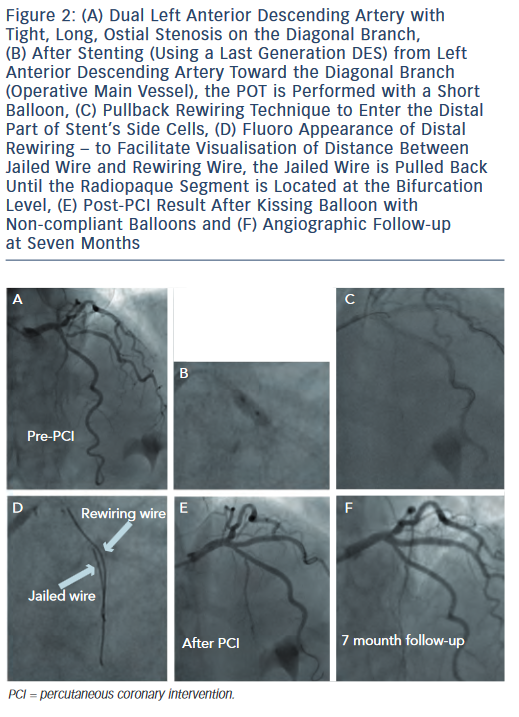 the systematic provisional approach, careful evaluation of the operative MV axis is mandatory. Indeed, when treating a bifurcated lesion with a single stent, it is pivotal to cover as much as possible the atherosclerotic disease with the stent. An example of provisional stenting with inverted operative MV axis is shown in Figure 2. When adopting this strategy (i.e. use of distal SB for first stent implantation), it is advisable to carefully evaluate the bifurcation anatomy by invasive imaging (intravascular ultrasound or optical coherence tomography [OCT]) in order to ascertain the pre-intervention plaque distribution pattern and the result obtained.
the systematic provisional approach, careful evaluation of the operative MV axis is mandatory. Indeed, when treating a bifurcated lesion with a single stent, it is pivotal to cover as much as possible the atherosclerotic disease with the stent. An example of provisional stenting with inverted operative MV axis is shown in Figure 2. When adopting this strategy (i.e. use of distal SB for first stent implantation), it is advisable to carefully evaluate the bifurcation anatomy by invasive imaging (intravascular ultrasound or optical coherence tomography [OCT]) in order to ascertain the pre-intervention plaque distribution pattern and the result obtained.
Similarly, when dealing with diffuse disease in both MV and SB, the operative MV axis should take into account the easiness of SB rewiring. Accordingly, in case of prohibitive SB take-off with high probability of suboptimal result, it is advisable to accept the possibility to end up with double stenting and to facilitate this by implanting the first stent toward the SB.
For provisional stenting, it should be recognised that the MV stent selection is of crucial importance to guarantee a satisfactory final result. Indeed, MV stenting may induce a significant worsening at the level of jailed SB. Recent data have demonstrated that this phenomenon is mainly related to the so-called 'carina shift (shift of the highly mobile soft tissue located at the flow divider) rather than to plaque shift.8,9 As a consequence, MV stent oversizing in the critical area of the carina (i.e. the segment of MV located immediately after the SB take-off) should be avoided, especially when dealing with acute angles. Accordingly, we use to select the MV stent diameter on the basis of the distal MV diameter. This causes a systematic malapposition of the stent at the level of proximal MV that must be promptly corrected by post-dilating the proximal part of MV stent with appropriately sized balloons according to the proximal optimisation technique (POT).10 Regarding the POT, the technical characteristic of the different DES should be considered. Indeed, DES response to the POT has been recently recognised to be highly variable. In particular:
 cells after the POT; as a consequence, when performing the POT, some DES may have an higher side cell opening in front of the SB take-off.12
cells after the POT; as a consequence, when performing the POT, some DES may have an higher side cell opening in front of the SB take-off.12Careful attention is also mandatory when selecting the length of the MV stent as well as the length and position for post-dilating balloon. Indeed, it is important to cover at least 6-8 millimetres (mm) of the proximal MV segment with the stent. Such length is needed to accommodate the shorter available balloon for the POT in order to avoid any injury to the proximal stent edge. Regarding the balloon selection for the POT, it should be short enough to not exceed the proximal edge of the stent and to avoid touching the distal MV in order to avoid carina shift. Of note, while performing the POT, we select non-compliant balloons only when MV stent under-expansion is due to highly resistant fibrotic or calcified plaque. In the remaining cases, we choose semi-compliant balloons to take advantage of balloon compliance to fully appose the stent struts toward the vessel wall (see Figure 3 for OCT documentation of full apposition of a last generation DES in a large left main).
Beside carina and plaque shift, it should be recognised that the SB patency after MV stenting is dependent on a complex interplay between bifurcation geometry and its deformation induced by stent.13 As a consequence, during bifurcation interventions with provisional approach, the risk of SB compromise should be strongly considered. Even if the jailed guidewire technique has been proven to be effective in facilitating bifurcation interventions,14 in some situations the risk of SB occlusion may be predicted to be very high. In these conditions, the protection of the SB may be further enhanced using the jailed balloon protection technique.15 According to this technique, an uninflated balloon is kept in the SB during MV stenting.15 It is then removed uninflated in case of SB Thrombolysis In Myocardial Infarction (TIMI) grade 3 flow or it is inflated to restore SB flow in the case of its occlusion.15 Such technique has been reported to allow treating safely patients with adverse bifurcation anatomies.15,16