Results
Several observational series have now been published describing the results of hybrid valve/PCI procedures. In a series reported by Byrne et al. of 26 patients with an average estimated Society of Thoracic Surgeons risk of mortality of 22 %, hybrid AVR and 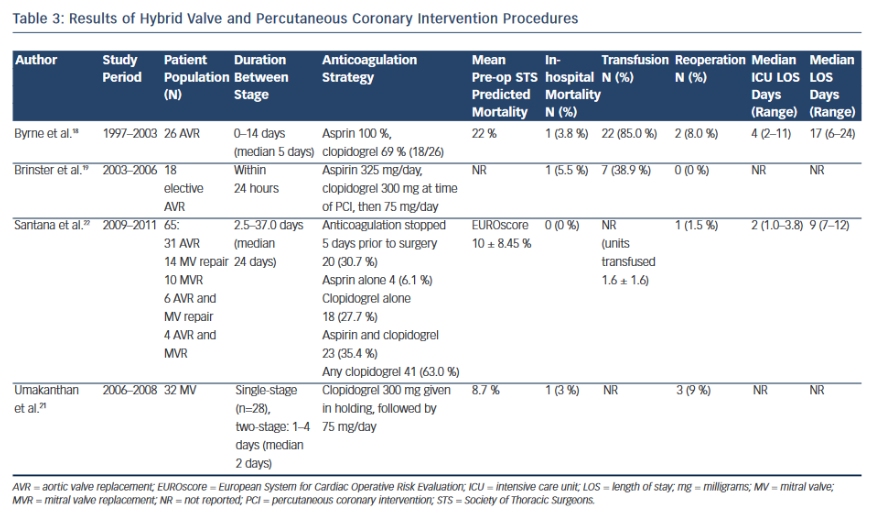 PCI proved feasible and safe with operative mortality in only one of the 26 patients (3.8 %).18 In this series, the surgical valve replacement was performed as a staged procedure, on average five days after the PCI. All patients were treated with aspirin and 69 % received clopidogrel at the time of operation. However, the series was largely dominated by high-risk patients presenting in cardiogenic shock secondary to myocardial infarction, and an increase in peri-operative blood loss and transfusion requirements were observed, mitigating some of the benefit of the hybrid approach. (See Table 3).
PCI proved feasible and safe with operative mortality in only one of the 26 patients (3.8 %).18 In this series, the surgical valve replacement was performed as a staged procedure, on average five days after the PCI. All patients were treated with aspirin and 69 % received clopidogrel at the time of operation. However, the series was largely dominated by high-risk patients presenting in cardiogenic shock secondary to myocardial infarction, and an increase in peri-operative blood loss and transfusion requirements were observed, mitigating some of the benefit of the hybrid approach. (See Table 3).
Brinster et al. reported a prospective observational series of 18 patients who underwent hybrid AVR and PCI.19 All patients who underwent PCI were treated with aspirin 325 mg and clopidogrel 300 mg initial load (followed by 75 mg daily), and PCI was followed by within 24 hours. In this series, one operative death occurred, but no late deaths were seen at up to 19 months of follow-up. There were no reoperations for bleeding and blood loss was minimal with mean transfusion of packed red blood cells less than one unit. In addition to decreased transfusion rates, this hybrid strategy was associated with a decreased length of stay.
Subsequently, Santana et al. directly analysed the outcomes of a staged hybrid valve/PCI approach to that of traditional surgery.22 In a retrospective analysis of 65 consecutive, matched patients who underwent planned PCI followed within 60 days (median 24 days) byeither aortic and/or mitral valve surgery, there were no in-hospital deaths in the hybrid population, no difference in transfusion rates and no reoperations for bleeding.
Specific to mitral valve, Umakanthan et al. described the Vanderbilt experience with 32 consecutive patients who underwent a hybrid procedure, including PCI and mitral valve surgery. Of these procedures, 28 (89 %) were performed as a single-stage procedure in a hybrid operating room.21 The observed in-hospital mortality rate was 3 % (1/32) and survival at one and two years was 96 % and 89 %, respectively. The series was expanded to 39 patients and reported by Solenkova et al., noting a predicted mortality for conventional CABG/ mitral of 14.1 % versus an observed in-hospital mortality of only 2.6 % (1/39).10
Procedural Timing
The optimal relative timing of the staged hybrid valve/PCI procedures remains unknown. A one-stop, or single-stage procedure may be appealing with respect to convenience, patient safety and resource utilisation. However, the ability to perform a single-stage procedure may be limited by the availability of appropriate staff and facilities.23,24 The single-stage approach requires a hybrid suite that can accommodate the equipment to perform the PCI as well as full cardiopulmonary bypass-based cardiac surgery; this includes general anaesthesia, transoesophageal echocardiography, the perfusion team and the cardiopulmonary bypass machine, in addition to the standard operating team and equipment. The risk-benefit profile of a single-stage procedure may also become unfavourable in the setting of significant renal dysfunction and certain other clinical circumstances. Finally, the management of required antiplatelet and anticoagulation therapies may be challenging based on the relative timing of the hybrid procedures.
Anticoagulation Management
Regardless of the hybrid strategy employed, concern remains over the impact of clopidogrel, or other antiplatelet therapies, at the time of cardiac surgery. The early hybrid experience was associated with increased blood loss and higher transfusion rates, which was attributed to the use of clopidogrel at the time of the valve operation.18 The subsequent strategy of shortening the duration between stages offered the potential to circumvent the increased risk of bleeding based on the pharmacokinetics of clopidogrel. However, more contemporary data suggests the risk of surgical bleeding while on clopidogrel may be overestimated.25
Furthermore, the risk of bleeding may be significantly reduced with the introduction of novel anticoagulants and antiplatelet agents. Cangrelor (The Medicines Company, Parsippany, New Jersey, US), an intravenous adenosine diphosphate receptor antagonist with a short half-life and rapid onset, has been shown to be safe and effective during PCI. The Cangrelor versus Standard Therapy to Achieve Optimal Management of Platelet Inhibition (CHAMPION) PHOENIX trial was a recently published, double-blinded, placebo-controlled trial of 11,145 patients undergoing urgent or elective PCI.26 The use of cangrelor was associated with a reduction in the rate of ischaemic events, including stent thrombosis, without an increase in severe bleeding. Although the effect of cangrelor in surgical patients is unknown, an intravenous antiplatelet agent with rapid onset that could be administered precisely at the time of PCI might prove to be highly beneficial with respect to the hybrid PCI/valve procedure.
Cost-effectiveness
In the current era of closely scrutinised healthcare spending, the cost-effectiveness of hybrid procedures must be further evaluated prior to broad adoption. The available literature suggests the hybrid valve/PCI approach is safe and effective, and may be associated with lower blood transfusion rates, shorter lengths of stay, and ultimately lower cost.5,9,19,20 Further cost savings may be realised by implementation of a single-stage approach, since only one hybrid suite and personnel team are utilised. Further study is necessary to truly delineate the cost-effectiveness of the hybrid valve/PCI approach.
Transcatheter Valve Replacement and Percutaneous Coronary Intervention
Fully transcatheter approaches to valvular and coronary heart disease, including PCI and transcatheter aortic valve replacement (TAVR), are beyond the scope of this review.27 However, a truly hybrid strategy involving open surgery and TAVR has been proposed as a means of addressing aortic stenosis and CAD (particularly LAD lesions) in a patient who is inoperable due to anatomic factors, such as hostile chest, porcelain aorta, complex reoperation, or patent right internal mammary artery crossing anterior to the aorta. The hybrid strategy in this regard combines a TAVR (transfemoral, transapical or transaortic) and open or minimally invasive direct coronary bypass grafting through a left mini-thoracotomy.28-35 Further study is necessary to better understand the risks and benefits of this new hybrid approach.