Microvascular vs Macrovascular Reperfusion- Implications on Clinical Reperfusion
Patency in Infarct-related Artery After Acute Myocardial Infarction and Outcome
Previously, patency of infarct-related artery after thrombolysis has been defined by the Thrombolysis in myocardial infarcti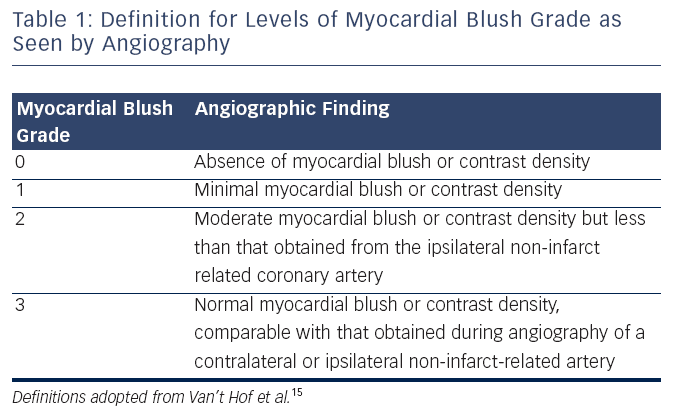 on (TIMI) research group.16 The TIMI system grades antegrade flow seen angiographically. Grade 0 denotes no perfusion as seen by absence of contrast flow through stenosis.16 Grade 1 flow means there is contrast seen through stenosis but the artery fails to completely fill the entirety of the artery.16 Grade 2 flow indicates complete filling of the artery with contrast past the stenosis but the rate of flow is less than that seen in a normal artery, or contrast clearance is delayed compared to that seen in a normal artery.16 Grade 3 indicates that artery fills and clears of contrast completely at a rate comparable to a normal artery.16 The open artery hypothesis that relates an improvement in survival to establishing normal flow in the IRA and hence patency of the artery has been demonstrated in previous studies.17 TIMI grade 3 is associated with a marked reduction in 30-day mortality, with an odds ratio of 0.44 (95 % CI, 0.24 to 0.79).17 There appears to be stepwise improvement in outcomes with ranging from TIMI 0–3 after primary PCI.15,18 However, TIMI flow as a prognostic tool after PPCI is less useful because more than 90 % of patients have TIMI 3 flow at end of PPCI.15
on (TIMI) research group.16 The TIMI system grades antegrade flow seen angiographically. Grade 0 denotes no perfusion as seen by absence of contrast flow through stenosis.16 Grade 1 flow means there is contrast seen through stenosis but the artery fails to completely fill the entirety of the artery.16 Grade 2 flow indicates complete filling of the artery with contrast past the stenosis but the rate of flow is less than that seen in a normal artery, or contrast clearance is delayed compared to that seen in a normal artery.16 Grade 3 indicates that artery fills and clears of contrast completely at a rate comparable to a normal artery.16 The open artery hypothesis that relates an improvement in survival to establishing normal flow in the IRA and hence patency of the artery has been demonstrated in previous studies.17 TIMI grade 3 is associated with a marked reduction in 30-day mortality, with an odds ratio of 0.44 (95 % CI, 0.24 to 0.79).17 There appears to be stepwise improvement in outcomes with ranging from TIMI 0–3 after primary PCI.15,18 However, TIMI flow as a prognostic tool after PPCI is less useful because more than 90 % of patients have TIMI 3 flow at end of PPCI.15
Microvascular Perfusion
There has been increasing focus on looking beyond flow in infarct artery to microvascular perfusion. ST resolution (STR) is considered a non-invasive measure of tissue perfusion.15 After PPCI, it has been shown that there was a reduction of mortality with more complete STR – in those with absent STR (<30 %) the mortality rate is 8.4 % whereas tho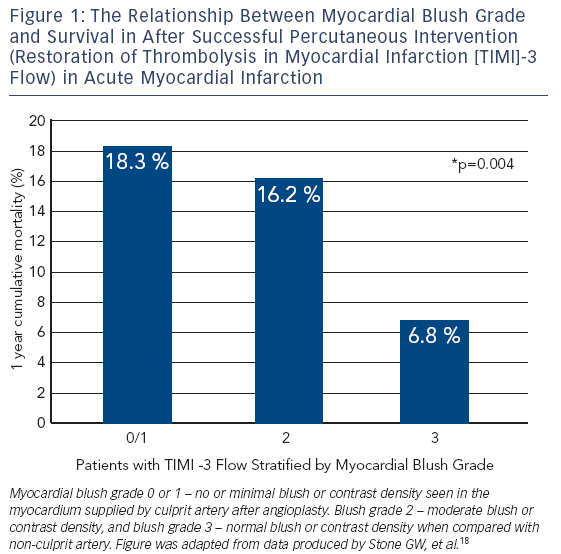 se with partial STR (30–70%) and complete STR (>70 %) have a mortality of 5.0 and 5.6 % respectively.19
se with partial STR (30–70%) and complete STR (>70 %) have a mortality of 5.0 and 5.6 % respectively.19
Microvascular flow can also be assessed by the myocardial blush grade (MBG), an angiographic measure of microvascular perfusion. As shown in (see Table 1) MBG is graded from 0 (absence of blush) to 3 (normal myocardial blush). Blush assessment requires a longer than average cine run to determine if blush clears.15
MBG has been shown to be an independent predictor of ST segment resolution, Killip Class after primary PCI and mortality.15 Compared to MBG of three, an MBG of zero or one has an eight-fold higher risk of long-term mortality (3 vs 23 % at two years, p< 0.0001).15 Interestingly, in the same study up to 67 % of patients with TIMI 3 flow had MBG of 0 or 1 which again suggests that epicardial blood flow does not necessarily imply tissue level perfusion.15 Even among those with TIMI 3 flow after angioplasty, an MBG grade of 0 or 1 may be associated with an increase for mortality (relative risk 4.7; 95 % CI 2.3 to 9.5; p< 0.001) (see Figure 1).18,20 This data has led to new paradigm that TIMI 3 flow is not enough; we must find methods to improve microvascular perfusion during PPCI.
Abnormal tissue perfusion in the presence of a patent epicardial artery is a phenomenon which is referred to as “No Reflow”.6 TIMI flow of less than three after an artery has been opened during PPCI is the most common finding which can be associated with no reflow. It is also an independent predictor of long-term cardiac death (relative risk [RR] 5.25, 95 % confidence interval [CI] 1.85 to 14.9, p=0002).21