In Vivo Evaluation
Systematic evaluation of side branches ≤2 mm jailed by the ABSORB BVS was performed by Okamura et al.17 Furthermor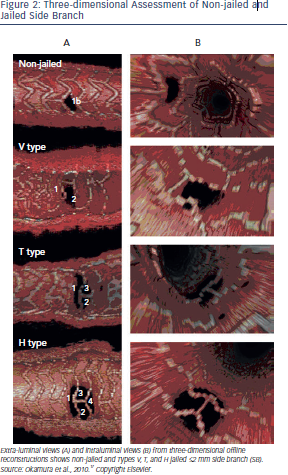 e, few case reports described the treatment of true bifurcations lesions with involvement of SB ≥2 mm.18–21 To allow full assessment of the ABSORB BVS SB struts, optical coherence tomography (OCT) was used in all these reports. OCT allows visualisation of the vessel wall and the ABSORB BVS struts at high resolution22 and with a high degree of reproducibility.23
e, few case reports described the treatment of true bifurcations lesions with involvement of SB ≥2 mm.18–21 To allow full assessment of the ABSORB BVS SB struts, optical coherence tomography (OCT) was used in all these reports. OCT allows visualisation of the vessel wall and the ABSORB BVS struts at high resolution22 and with a high degree of reproducibility.23
Okamura et al. assessed jailed side branch struts at baseline with three-dimensional (3D) OCT reconstruction, allowing the SB orifices to be evaluated visually. In total, 40 SB ostia of 25 patients enrolled in the ABSORB Cohort B study were analysed. In total, 24 orifices were jailed and showed different degrees and patterns of compartmentalisation (Type V, T and H) (see Figure 2).
Further insight in the use of the ABSORB BVS in coronary artery bifurcation lesions emerges from case reports combined with OCT images. Okamura et al. described a patient with an obstructed SB of ≤2 mm. Serial OCT imaging was performed at 2-year follow up showing an open SB ostium with intimal bridges creating a neocarina, persisting after absorption of the scaffold.24 Van Geuns et al. demonstrated the feasibility of crossing the ABSORB BVS struts into the SB with a coronary guidewire after deployment of a 3.0x18 mm ABSORB BVS in a left anterior descending (LAD) artery bifurcation lesion (Medina classification 1,1,0).21 Gogas et al. were first to describe side branch balloon dilatation of a LAD/second diagonal bifurcation lesion (Medina 1,1,1) treated wit h a single ABSORB BVS in the main branch. After deployment of a 3.0x18 mm ABSORB BVS in the midLAD, there was impaired flow and pinching of the ostium of the second diagonal, after which the scaffold was fenestrated towards the SB and dilated with a 1.5x12 mm Trek-compliant balloon. 2D OCT images and offline 3D-OCT reconstructions showed an open ostium of the SB and well-apposed struts in the SB segment.20 Finally, Grundeken et al. showed a successful deployment of a 3.5x18 mm ABSORB BVS in the left main coronary artery (LMCA) in the direction of the LAD, crossing the left circumflexus artery (LCx). However, after placement of the scaffold plaque shift towards the ostium of the LCx was observed on angiography. Therefore, the BVS was fenestrated towards the LCx and the LCx ostium was dilated with 2.0x20mm and 2.5x15mm Sapphire II compliant balloons at 8 atmospheres. Offline 3D-OCT reconstructions of the scaffold before fenestration showed multiple struts jailing the ostium of the LCx. After dilatation of the LCx ostium there is an opening of the stent cell seen towards the LCx without scaffold disruption (see Figure 3). These case reports illustrated that implantation of the ABSORB BVS and scaffold fenestration towards the SB with subsequent SB post-dilatation is feasible. Furthermore, these cases described the role of OCT to guide optimal scaffold placement.
h a single ABSORB BVS in the main branch. After deployment of a 3.0x18 mm ABSORB BVS in the midLAD, there was impaired flow and pinching of the ostium of the second diagonal, after which the scaffold was fenestrated towards the SB and dilated with a 1.5x12 mm Trek-compliant balloon. 2D OCT images and offline 3D-OCT reconstructions showed an open ostium of the SB and well-apposed struts in the SB segment.20 Finally, Grundeken et al. showed a successful deployment of a 3.5x18 mm ABSORB BVS in the left main coronary artery (LMCA) in the direction of the LAD, crossing the left circumflexus artery (LCx). However, after placement of the scaffold plaque shift towards the ostium of the LCx was observed on angiography. Therefore, the BVS was fenestrated towards the LCx and the LCx ostium was dilated with 2.0x20mm and 2.5x15mm Sapphire II compliant balloons at 8 atmospheres. Offline 3D-OCT reconstructions of the scaffold before fenestration showed multiple struts jailing the ostium of the LCx. After dilatation of the LCx ostium there is an opening of the stent cell seen towards the LCx without scaffold disruption (see Figure 3). These case reports illustrated that implantation of the ABSORB BVS and scaffold fenestration towards the SB with subsequent SB post-dilatation is feasible. Furthermore, these cases described the role of OCT to guide optimal scaffold placement.
Practical Recommendations
Although more clinical studies are needed to verify the optimal strategy in bifurcation lesions using ABSORB BVS, we would like to make the following recommendations based on previously described data and our own experience. In accordance with the recommendation of the European Bifurcation Club, based on randomised data on one- versus two-stent techniques using metallic stents, we would recommend the provisional single stenting technique in the majority of the lesions (see Figure 4), as previously suggested by D┼¥avík and Colombo.15
Adequate lesion preparation and optimal sizing of the ABSORB BVS is essential prior to scaffold placement. Stent sizing with metallic stents is recommended to be based on the distal diameter with subsequent postdilatation of the proximal main branch with a larger balloon to ensure stent apposition in the proximal main branch (proximal optimisation technique [POT]).25 This technique is considered to prevent carinal shift and subsequent ostial pinching of the SB. However, postdilation of the BVS with balloons >0.5 mm larger than the BVS size is discouraged due to the increased risk of strut f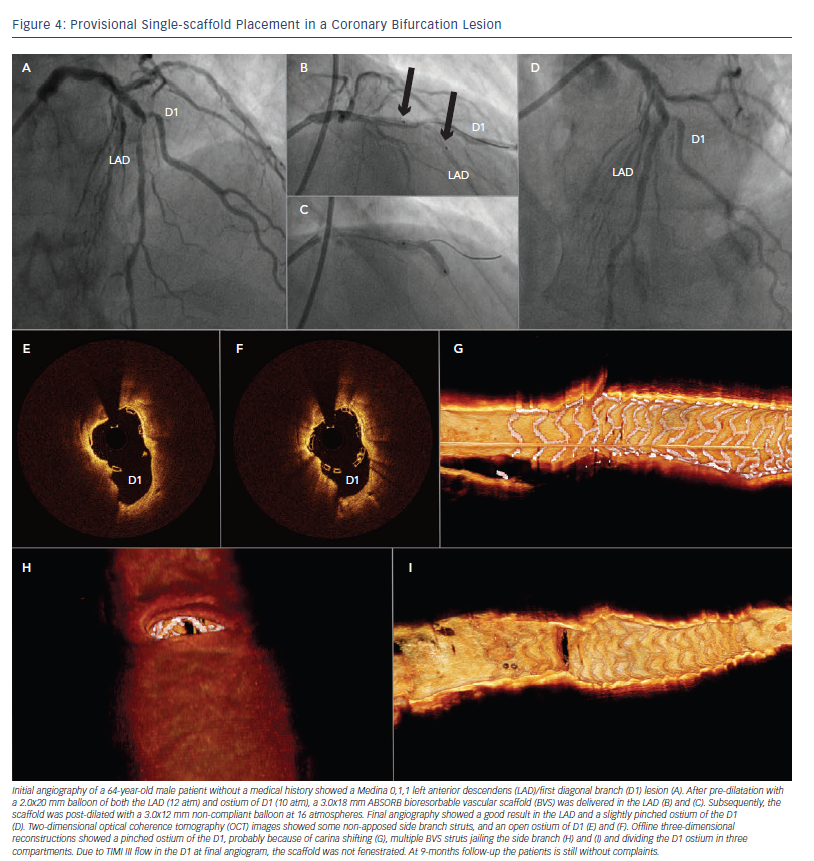 ractures. Therefore, we recommend to choose the BVS size based on the proximal diameter. Intravascular imaging, such as intravascular ultrasound (IVUS) or OCT, or online quantitative coronary angiography (QCA) can be used for optimal sizing of the ABSORB BVS.
ractures. Therefore, we recommend to choose the BVS size based on the proximal diameter. Intravascular imaging, such as intravascular ultrasound (IVUS) or OCT, or online quantitative coronary angiography (QCA) can be used for optimal sizing of the ABSORB BVS.
After deployment of the scaffold, we recommend to guide further need for fenestration and post-dilatation of the scaffold on the angiographic result and OCT images. If a lesion after deployment of the scaffold has a severely pinched ostium on angiography combined with impaired flow, Thrombolysis In Myocardial Infarction (TIMI) flow 1 or 2, we recommend the fenestration of the scaffold towards the SB. Online 3D-OCT reconstructions, which are available at the newest OCT consoles, could guide the optimal guidewire position during recrossing towards the SB. Recrossing through the most distal compartment is recommended, as distal recrossing leads to a reduction of incomplete stent apposition (ISA) at baseline in metallic stents.26 In our experience, fenestration of the scaffold towards the SB is feasible with a 2.0 mm or a 2.5 mm balloon in the SB ostium to a maximum of 6 to 8 atmospheres. Final OCT pullback after fenestration could be performed to detect whether the scaffold is well apposed in the whole stented area and to control for any struts out of the expected range. The latter is a sign of strut fracture, which could be treated with additional stenting. Due to lack of clinical data, we recommend repeat angiography to be performed combined with OCT at 9 months after scaffold placement, even if the patient is without any complaints. This allows assessment of the TIMI flow in the SB and MB, intimal tissue bridging in front of the SB and intimal formation in the distal MB. Treatment of ABSORB BVS re-stenosis has not been investigated in clinical trials; however, Nakatani et al. showed a case series of six patients with in-stent restenosis who have been treated with additional stenting using Xience drug-eluting stents.27