Malapposition After Stent Implantation
ISA after implantation is a relatively common finding by OCT. The high resolution of the technique allows the detection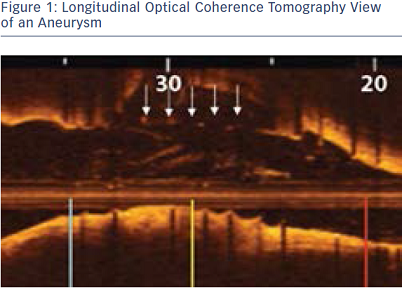 of very small areas of ISA or even single malapposed struts. The clinical significance of ISA as detected by OCT, however, is poorly understood, and there is no consistent data indicating when it would be necessary to correct it. From a clinical perspective, we could consider treating it only when the degree of malapposition is significant (e.g. affects various struts and extends longitudinally in several frames (see Figure 1).
of very small areas of ISA or even single malapposed struts. The clinical significance of ISA as detected by OCT, however, is poorly understood, and there is no consistent data indicating when it would be necessary to correct it. From a clinical perspective, we could consider treating it only when the degree of malapposition is significant (e.g. affects various struts and extends longitudinally in several frames (see Figure 1).
The presence of ISA is influenced by several factors, such as stent design, lesion characteristics (calcification, bifurcation, length of the lesion) and procedural technique (high-pressure implantation, pre-dilatation, post-dilatation). OCT could be useful to identify lesions with a high risk of ISA and guide the procedure strategy in order to minimise the risk (e.g. use rotational atherectomy in heavily calcified lesions) and optimize the final result (e.g. post-dilatation with a non-compliant balloon).
Malapposition at Follow-up
At follow-up, OCT can also assess the presence of ISA (which can be 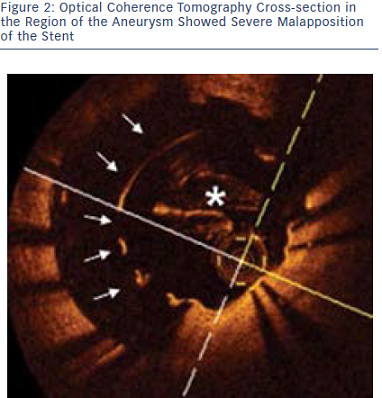 persistent or late-acquired) and provide insights into its mechanisms (see Figure 2). Persistent ISA is generally caused by stent underexpansion related to the presence of severe calcification. Another cause can be the apposition of the struts over an intimal dissection that does not heal at follow-up. Several causes of late-acquired ISA have been proposed and also can be evaluated with OCT:
persistent or late-acquired) and provide insights into its mechanisms (see Figure 2). Persistent ISA is generally caused by stent underexpansion related to the presence of severe calcification. Another cause can be the apposition of the struts over an intimal dissection that does not heal at follow-up. Several causes of late-acquired ISA have been proposed and also can be evaluated with OCT:
To be able to recognise persistent ISA and to identify chronic stent recoil, post-implantation and follow-up imaging would be required. Treatment of ISA detected with OCT at follow-up is only recommended if the cause is correctable and has induced a clinical problem (e.g. stent underexpansion in stent thrombosis).
The publication of this information was supported by St. Jude Medical.