Rationale for an Early Management of Shock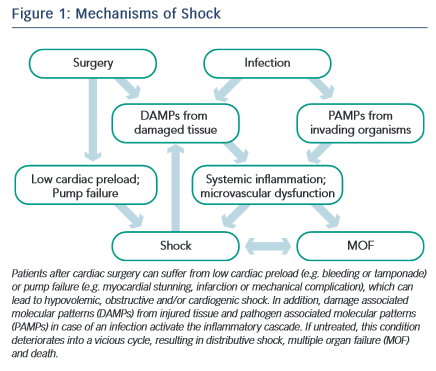
Shock in patients undergoing cardiac surgery occurs frequently with multiple potential causes at play.1,2 Figure 1 depicts the interactions between surgery, infection, the systemic inflammatory response syndrome (SIRS), shock and multiple organ failure. The time between shock onset and shock resolution is one factor that defines the degree of organ dysfunction and the risk of death, as prolonged shock causes inflammation and irreversible tissue damage.6 Hence, prompt identification of patients with shock and immediate treatment are crucial for the outcome of such patients. The concept of goal-oriented resuscitation was pioneered by Shoemaker et al in high-risk surgical patients.7 Rivers et al published in 2001 that early goal-directed therapy (EGDT) significantly reduced mortality in patients with septic shock.8 Kumar et al demonstrated that early administration of appropriate antibiotics in septic patients with hypotension saved lives in a time- dependent manner.9 Accordingly, guidelines were published for the initial management of patients with sepsis and septic shock.5 Several studies have demonstrated a survival benefit for patients if such guidelines were implemented in clinical practice.10–12 The idea of EGDT was expanded to the clinical scenarios of acute heart failure13 and heart failure after cardiac surgery.14
More than 10 years later three large multi-centre trials re-evaluated the results of River’s landmark study: ARISE, ProCESS and ProMise.15–17 In these trials EGDT was not superior to standard care in patients with early septic shock.18 This might be explained by the fact that the included patients were less ill than in the original study. Second, the standard care groups might have benefited from early recognition and treatment of septic shock that have become the standard of care over the past decade. Third, continuous measurement of central venous saturation is not necessary to guide treatment of pathophysiological deteriorations. However, when shock does not resolve promptly with standard therapy, echocardiography and invasive haemodynamic monitoring become necessary to unravel the complex underlying mechanisms and to decide on further treatment. These principles can be implemented for all forms of shock, as the underlying pathophysiologic mechanisms (tissue damage, release of damage-associated molecules, inflammation, organ dysfunction) are similar in different shock states.
Definition of Shock
Shock is defined by the presence of global tissue hypoperfusion and signs of organ dysfunction resulting from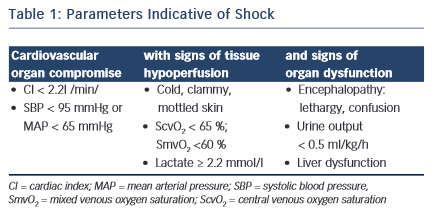 severe cardiovascular compromise. Common clinical, haemodynamic and laboratory parameters indicative of shock are displayed in Table 1 (adapted from Kumar and Parillo2).
severe cardiovascular compromise. Common clinical, haemodynamic and laboratory parameters indicative of shock are displayed in Table 1 (adapted from Kumar and Parillo2).
Four particular shock types can be distinguished (adapted from Kumar and Parillo2):
Diagnostic Assessment
Table 2 describes a structured approach to the patient in shock. Physicians must be aware that simplifying the diagnostic process (i.e. cutting corners) bears the risk of false interpretation, particularly as patients after cardiac surgery often have more than one possible cause of shock. A thorough understanding of the obtained results in the clinical context is more important than the performance of the test itself. All values have to be interpreted and immediately implemented in the therape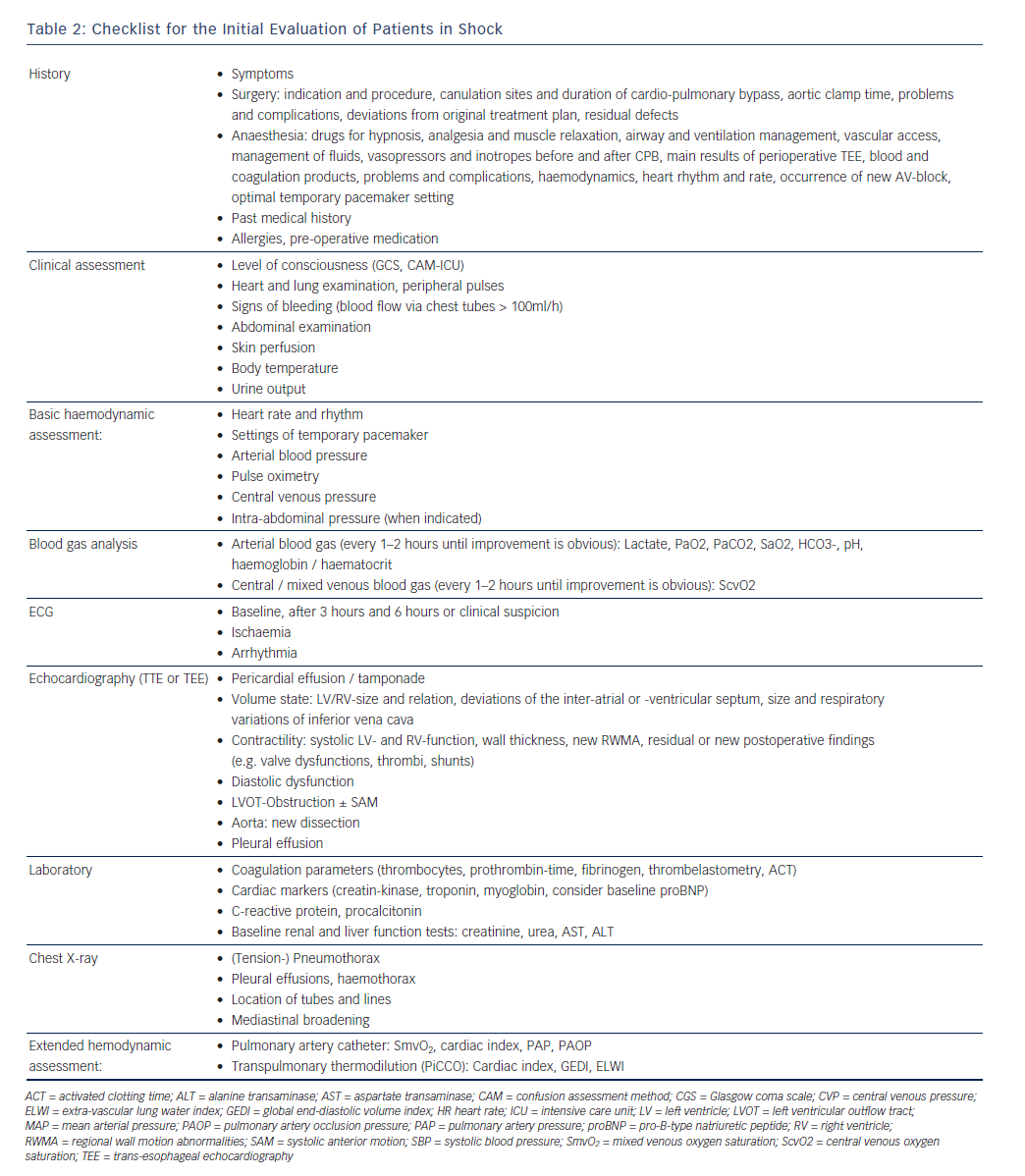 utic decision process.
utic decision process.
Echocardiography
A useful tool for the haemodynamic evaluation of patients with shock is echocardiography. It is readily available, non-invasive and can be performed after a reasonable period of training.19–21 However, expert advice should be available around the clock, as examination conditions in cardiovascular patients can be challenging (e.g. substernal air, dressings, chest tubes) and the underlying pathologies difficult to detect (e.g. localised pericardial effusion with tamponade, intracardiac shunts, dysfunction of artificial valves). If the quality of transthoracic imaging is insufficient, a transoesophageal echocardiography is indicated. Due to its semi-invasiveness complications may occur and contraindications should be respected. Oesophageal injury occurred in a single-centre study of 10,000 patients in fewer than one per 1,000 cases.21,22
Lactate
In hypoxic cells, glucose is metabolised to lactate, resulting in a much lower ATP yield as when glucose can be metabolised via pyruvate in the Krebs cycle under aerobic conditions. Therefore, lactate is a useful marker of an energy crisis at the cellular levels in patients with shock. Whereas in low-flow shock states a lactate elevation is often caused by tissue hypoxia, in distributive shock the mechanisms are more complex and involve the increase in glycolysis, inhibition of pyruvate dehydrogenase23 and the stimulation of muscular Na+/ K+ ATPase.24 High lactate plasma levels and insufficient lactate elimination are associated with poor outcome.25–27 Consequently, lactate has proved to be a useful parameter for evaluation of the resuscitation process of patients with septic shock.28 In the study by Jones et al, packed red blood cells were transfused if lactate clearance was <10 % within 1 hour and haematocrit was <30 %; dobutamine was initiated if lactated clearance remained low.29 Other investigators demonstrated a mortality-reduction in patients with a blood lactate level > 3mmol/l, when a decrease of 20 % in the blood lactate level over 2 hours was targeted.30 Nevertheless, because of its complex metabolism and physiology, elevated lactate levels per se are not an indication for the administration of fluids or inotropes; lactate values might change more slowly than other haemodynamic parameters of perfusion.
Importantly, lactate is also released by fully oxygenated tissues.31,32 The production is stimulated by adrenaline and lactate, in this case rather fuel than waste product, acts as an energy shuttle from skeletal muscles to vital organs, such as the heart and brain.33,34 In addition, lactate elevations may result not only from increased production but also from decreased elimination as in acute liver dysfunction. In conclusion, elevated lactate levels must be interpreted with caution as they do not in every case indicate tissue hypoxia.34,35