Treatment Recommendations
Once shock is identified, the most important goal is the correct diagnosis of the underlying cause and the mechanisms at play. Simultaneously, prompt resuscitation measures are undertaken to provide adequate oxygen delivery and to prevent further organ damage. Tissue oxyge nation is adequate when the balance between oxygen consumption and delivery is met. Treatment recommendations are summarised in Table 3. While there are clear differences in the treatment of cardiogenic shock and septic shock patients (e.g. revascularisation versus source control), there are also similarities (e.g. vasopressors in cases of decreased vascular tone).
nation is adequate when the balance between oxygen consumption and delivery is met. Treatment recommendations are summarised in Table 3. While there are clear differences in the treatment of cardiogenic shock and septic shock patients (e.g. revascularisation versus source control), there are also similarities (e.g. vasopressors in cases of decreased vascular tone).
Optimise preload
Fluid therapy is recommended to re-establish vascular filling and cardiac preload in patients with shock (Tables 3 and 4). However, despite considerable research efforts resulting in more than 4,000 articles (including more than 860 reviews) listed in PubMed.gov, the best fluid for shock resuscitation is still a matter of debate. Adverse effects and costs vary according to the fluids used, without clear benefit favouring one solution over others. A large observational study revealed, that gelatin 4 % solutions and hydroxyethyl starch (HES) 6 % (130/04) led to a similar dose-related increase of renal failure in critically ill patients.36 In contrast, fluid resuscitation with only crystalloids significantly reduced the incidence of acute kidney injury in severe sepsis patients.37 The 6S study showed increased mortality and need for renal replacement therapy in the HES group compared with the use of crystalloids.38 There is evidence that HES preparations are stored in human tissue and are associated with kidney failure,39,40 increased bleeding risk41 and higher mortality.39,42 Therefore, and because of the findings above, HES is no longer used in the Zurich ICU.
Large volume transfusion with 0.9 % saline may result in hyperchloremic metabolic acidosis.43 Additionally, studies show that the use of balanced salt solution, compared with 0.9 % saline, are associated with a decreased rate of infections, renal dysfunction, and blood transfusion.44–46
The SAFE study, a large multi-centre study comparing normal saline with albumin 4 % solutions, found a similar mortality with both solutions irrespective of baseline albumin concentrations.47,48 Post hoc analysis revealed a decreased mortality risk in the subgroup of septic patients49 when treated with albumin 4 %. In another study, albumin was associated with a lower mortality compared with other fluid regimens.50 In a retrospective study with almost 20,000 patients undergoing coronary artery bypass surgery, Sedrakyan et al compared the effect of different colloids on the postoperative mortality.51 Albumin was used in more than 8,000 patients and non-protein colloids (HES and dextran) in the rest of the cohort. The mortality rate was 25 % lower in patients receiving albumin. This difference might be explained by a better maintenance of vascular integrity during ischaemia-reperfusion,52 the reversal of hypoalbuminaemia (a strong risk factor for mortality),53 as well as by excessive bleeding associated with starches. Gelatin and HES reduced maximum clot firmness of thromboelastometry tracings, whereas these values remained unchanged after administration of albumin.54 The major disadvantages of current available human albumin solutions include high cost, it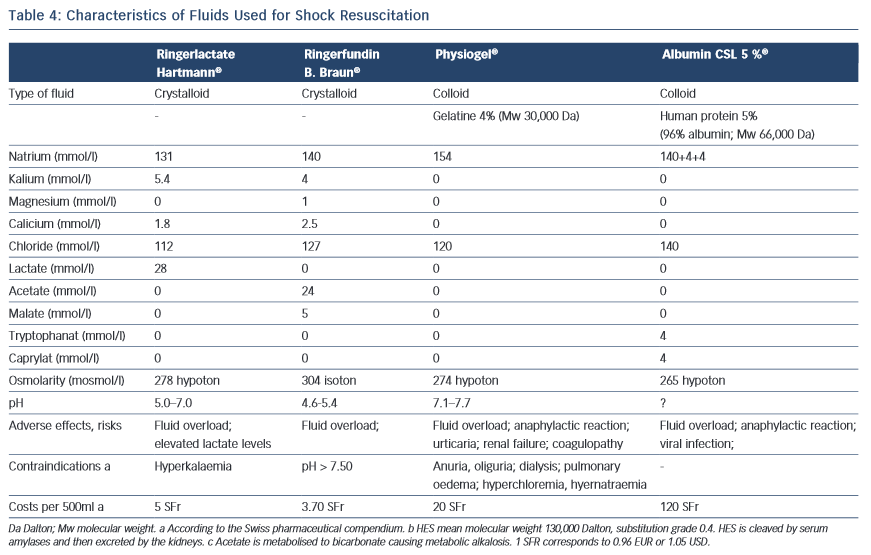 s delivery via glass bottles and the potential, although small, risk of viral infections. Taking these partly conflicting results into account, a fluid regimen as described in Table 3 is suggested. Details of the proposed fluids are summarised in Table 4.
s delivery via glass bottles and the potential, although small, risk of viral infections. Taking these partly conflicting results into account, a fluid regimen as described in Table 3 is suggested. Details of the proposed fluids are summarised in Table 4.
Maintain Perfusion Pressure
Providing an adequate perfusion pressure during shock by restoring (or increasing) blood pressure is a key intervention in the treatment of shock. Most reviews and guidelines recommend a target MAP of 65 mmHg.23,55
When hypotension persists despite a fluid challenge, vasopressors are started. Noradrenalin is used because of its -adrenergic and -adrenergic properties. stimulation increases vascular tone while stimulation improves contractility. Noradrenalin is the vasopressor of choice in septic shock5 as well as in other forms of shock. A limiting factor is excessive vasoconstriction and organ ischaemia, which is sometimes difficult to distinguish from ischaemia caused by inadequate resuscitation.56 Adrenalin can be used in acute life- threatening shock. At low doses, mainly -adrenergic effects are transmitted, while -adrenergic effects dominate at high doses. Important side effects of adrenalin are arrhythmias, metabolic effects (hyperglycaemia, hyperlactaemia) and a decrease in splanchnic blood flow, bearing the risk of mesenterial hypoperfusion.57,58
Vasopressin is used in patients with noradrenalin doses >0.5 mcg/kg/min. In septic shock, vasopressor deficiency can occur59 and its supplementation is safe60–62 with a catecholamine sparing effect.63 A survival benefit could not be shown for patients with mild septic shock and for those who received glucocorticoids.23,62,64 Patients with cardiogenic shock might even be harmed by the increase in afterload and the coronary vasoconstriction.65 In accordance with others, a maximum dose of 0,04 U/min is recommended.5,23
Methylene blue prevents vasodilation by inhibiting soluble guanylyl cyclase and nitric oxide synthase activity. The optimal dose is unknown,66 as well as its effect on morbidity and mortality.67 Methylene blue (2 mg/kg iv) in persistent shock should only be used during the first 24 hours following cardio-pulmonary bypass. It is worth noting, that the Surviving Sepsis Campaign does not mention methylene blue in its recommendations.5