Decision-making
Providers have varying degrees of comfort with the provision of end-of-life care in HF.6 At or near the end of life, 52 % of providers hesitated to discuss end-of-life care, due 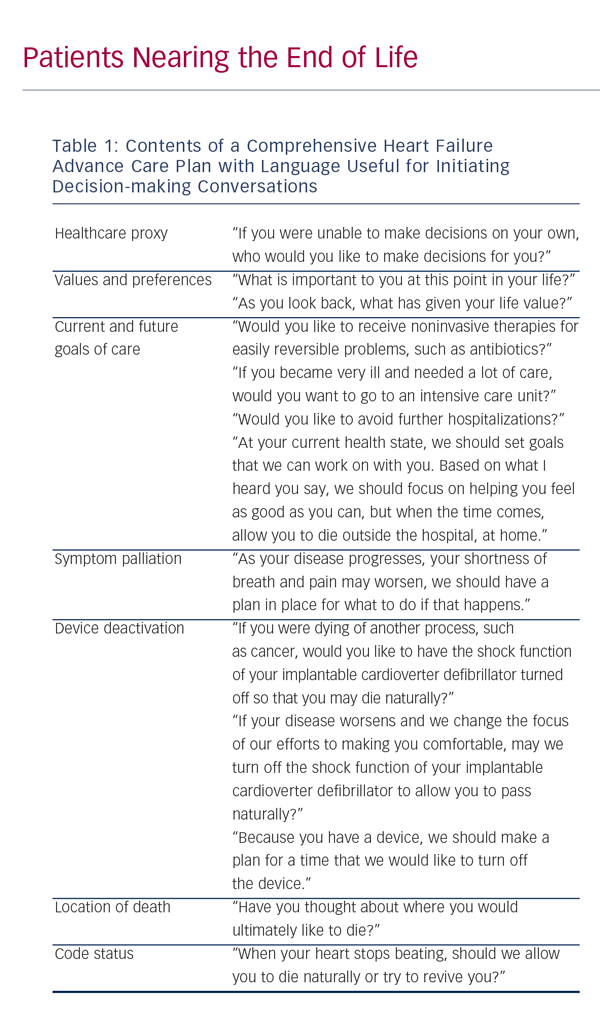 to provider discomfort (11 %), perceived unreadiness on behalf of the patient or family (33 %), fear of destroying hope (9 %), or lack of time (8 %). Furthermore, 30 % of these providers reported low or very low confidence in initiation of the discussions, enrolling in hospice, or providing end-of-life care. Opinions differ among providers about whose responsibility it is to address end-of-life care in patients with HF, with 66 % of cardiology providers citing that the responsibility is that of the primary care physician (PCP), while 57 % of PCPs believe the converse. We suggest that all providers should review preferences and planning for the end of life with HF patients and that any invested provider may initiate end-of-life care. Decision-making for end-of-life matters should be patient-centered and should be a collaborative effort between providers, patients, and involved family and friends of the patient. The decisions needing to be made at the end of life generally fall under the umbrella of an advance care plan (ACP).
to provider discomfort (11 %), perceived unreadiness on behalf of the patient or family (33 %), fear of destroying hope (9 %), or lack of time (8 %). Furthermore, 30 % of these providers reported low or very low confidence in initiation of the discussions, enrolling in hospice, or providing end-of-life care. Opinions differ among providers about whose responsibility it is to address end-of-life care in patients with HF, with 66 % of cardiology providers citing that the responsibility is that of the primary care physician (PCP), while 57 % of PCPs believe the converse. We suggest that all providers should review preferences and planning for the end of life with HF patients and that any invested provider may initiate end-of-life care. Decision-making for end-of-life matters should be patient-centered and should be a collaborative effort between providers, patients, and involved family and friends of the patient. The decisions needing to be made at the end of life generally fall under the umbrella of an advance care plan (ACP).
Realistically, a large number of patients will die without either a well-thought-out ACP and signed advance directive (AD), however, the exercise of going through these questions with patients may help them to formulate opinions regarding their end-of-life care. Having an ACP and AD can help to alleviate anxiety, increase hospice utilization, and decrease the use of life-prolonging and invasive therapies at the end of life.7 The first step in helping a patient to create an ACP is to understand the patient’s goals and values. The next step is to inform the patient that they are nearing the end stage of the disease process and review reasonable treatment options in the context of their stated values and goals. Specific topics that should be addressed in a complete ACP, as well as useful language, are found in Table 1. Importantly, the ACP should be an iterative process, and should be readdressed throughout the course of illness, as patient preferences can change as their illness worsens.8
The use of device-based therapies, such as implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy, for HF is becoming integrated into the care of a greater percentage of patients, with over 50 % of patients with HF qualifying for device-based therapy.9 Challenges encountered by providers initiating conversations regarding device deactivation can be due to provider discomfort, lack of counseling prior to implantation, and patient misconceptions.10–12 However, ICD discharges at the end of life are associated with pain and anxiety at the end of life and should be averted. To that end, a plan should be in place for device deactivation for every patient. Planning for device deactivation should start before implantation, but findings from the Multicenter Automatic Defibrillator Implantation Trial II (MADITII) cohort suggest that using clinical status changes (such as hospitalization or changes in functional status) to prompt discussion regarding deactivation may not expose the patient to additional risk for shocks at the end of life.13 Deactivation of mechanical circulatory support is equally important to plan for, but will not be discussed in this review.
Symptom Management
Patients with HF nearing end of life are likely to encounter worsening of symptoms or development of new symptoms. The goal of palliative care is to lessen suffering in all forms: physical, psychological, social, or existential; recognition of each of these forms of suffering as a contributor to suffering is called the theory of “total pain.”1 A comprehensive approach to care addresses each of these forms of suffering in the dying patient. Whereas the transition to palliative care in other disease processes is marked by the removal of potentially curative or otherwise aggressive therapies, the transition to palliative care in those with HF should be additive.14 The key is to medically optimize to the fullest extent achievable with guideline-based medical therapy and then to add therapies directed at the underlying root cause of symptoms that are still present after traditional medical therapy has been exhausted.15
As patients with end-stage HF experience a high burden of symptoms, a multidisciplinary care team may be beneficial.16 This team usually involves both a PCP and a cardiologist, social work, nursing staff, and also, perhaps, a palliative care specialist. A randomized study of 232 patients admitted with HF at a tertiary referral center found that inpatient palliative care consultation improved symptoms burden (p<0.001) and quality of life (p<0.001) at serial follow-up.17