How to Plan an ET Programme
Exercise intensity for an ET programme may be planned by indirect exercise intensity assessment or through a direct identification of exercise intensity domain by gas exchange analysis through cardiopulmonary exercise testing (CPET). Even when exercise intensity is indirectly estimated, measurement of VO2 by CPET should be considered.5–7
The most common and widely applied indirect method for ET prescription is based on heart rate (HR), which is used as a reference variable assuming that the relationship 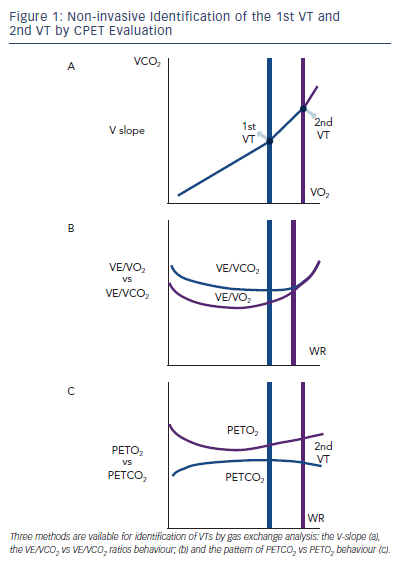
An important concept when using HR for exercise prescription is the concept of HR reserve (HRR), defined as the difference between HR at rest and peak exercise. An HRR percentage equal to 60 % has been identified as corresponding at the first ventilatory threshold (1st VT) in both normal and HF patients (see Figure 1).10 Practically, ET sessions for cardiac patients are proposed at a range of 40–70 % HRR.11 Another indirect parameter proposed by the most recent joint position statement 7 for planning ET programmes, is the VO2 reserve calculated as: (peak VO2-rest VO2) x (% intensity desired) + rest VO2. VO2 reserve provides an indicator of exercise intensity by reflecting the true amount of energy for maximal exercise attainment, taking into account baseline levels.7
In order to optimise ET prescription, a comprehensive use of CPET-derived information is highly suggested for a pathophysiologically and clinically precise determination of ET intensity level. A range of aerobic exercise testing, from light- to moderate- to high- to severe-intensity aerobic training, have been used with HF patients with variable effectiveness, according to patients’ characteristics and predefined target of intervention.12,13 The simpler and more effective way to plan ET programmes of mild to moderate intensity is the assessment of VO2 at the first ventilatory threshold, that is the metabolic condition above which blood lactic acid and pH starts to increase and decrease, respectively, generating a HCO3 buffering of the incoming acidosis. The 1st VT can be determined by three CPET-derived methods. The first is the V-slope, the point at which the incremental VCO2 production becomes higher than VO2 due to the additional CO2 produced by lactic acid buffering (see Figure 1a) with a slope of less than one to greater than one. There are two other gas exhange derived methods. One relies on the pattern of changes in ventilation (VE) to carbon dioxide (VCO2) production and VE to VO2 ratios, identifying the point of continuous increase in VE/VO2 and stable VE/VCO2 kinetics (see Figure 1b). The other is based on the definition of the point of divergent kinetics of the end-tidal partial pressure (PET) of CO2 vs the PETO2 (see Figure 1C).5
With increasing exercise intensity and lactic acid production above the 1st VT a second point is reached when bicarbonates no longer adequately compensate for metabolic acidosis.
This is the second ventilatory threshold (2nd VT) (see Figure 1a) and is when hyperventilation occurs and ventilatory alkalosis develops. At this stage the VE/VCO2 ratio increases and inverts its trend and PETCO2 decreases (see Figure 1 b,c).
The 1st VT signals the limit between mild-to-moderate and the moderate-to-high intensity domains corresponding to around 50–60 % of peak VO2 and 60–70 % of peak HR. Admittedly, in advanced HF and in a rate of approximately 20 %, VO2 at 1st VT cannot be determined. When identifiable, the 2nd VT is usually attained at around 70–80 % peak VO2 and 80–90 % peak HR reached during incremental exercise.
It is unknown if these methods can be interchangeably applied to ET programme prescriptions in the HF setting.
It has also to be considered that VO2 at 1st VT may be affected by the type of exercise; use of a treadmill leads to a 10 % higher peak VO2 compared to bike. Thus, ET programmes should be promoted and performed with the same modality with which they are planned.14 Despite these caveats, there is evidence that ET programmes based on VO2 at 1st VT compared to HRR method provide significantly higher improvements in peak VO2 and cardiac output as assessed by O2 pulse.15
The recent joint position statement of the European Association for Cardiovascular Prevention and Rehabilitation, the American Association of Cardiovascular and Pulmonary Rehabilitation and the Canadian Association of Cardiac Rehabilitation provides directions on the identification of ET intensity domains by using constant WR exercise tests, and looking at the different VO2 on kinetics response,7 which – though in most cases is impractical – remains the most accurate physiology-based approach. Briefly, VO2 kinetics during constant WR exercise reflects three phases of adaptation of the organ systems and factors involved in alveolar-to-cell O2 coupling: phase I, or cardiodynamic, during which the increase in VO2 is mediated by the immediate increase in cardiac output and pulmonary blood flow at the start of exercise; phase II, or cell respiration, reflecting decreased O2 content (muscle 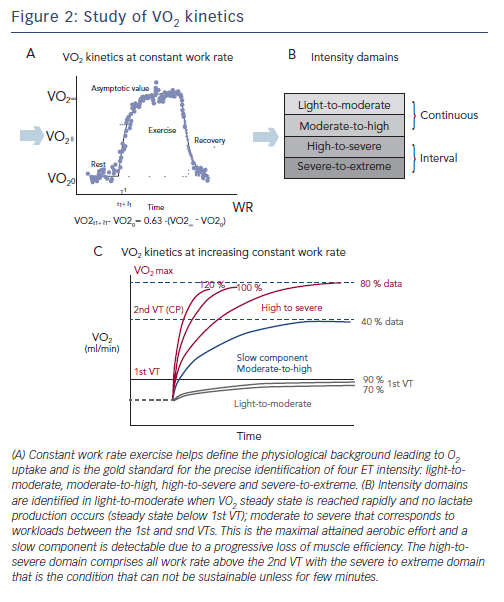
Light-to-moderate and moderate-to-high intensity programmes comprise continuous exercise, a condition that is not sustainable for high-to-severe and severe-to-extreme protocols requiring an interval exercise approach. Light-to-moderate intensity domains encompass the corresponding WR that engender a VO2 steady-state value below the corresponding 1st VT (see Figure 2c). During this WR and in this domain, a VO2 steady state is attained relatively rapidly following the commencement of exercise and there is no lactate production. For this reason, exercise can be well-tolerated and is generally sustainable for longer periods of time (30–40 min) with only a mild sense of fatigue and breathlessness.
The moderate-to-high intensity domain corresponds to those workloads between the 1st and 2nd VTs. The 2nd VT represents the maximal WR sustainable in conditions of both VO2 and lactate steady state and are the highest limit of sustainable prolonged aerobic exercise in HF patients. This work intensity determines a slow component (see Figure 2c) increase of VO2 after 2–3 minutes of constant WR, a component that is not detectable during incremental exercise. Interestingly, the VO2 slow component elevates the VO2 above the level expected for a given WR, yielding a delayed attainment of the VO2 steady-state by 10–15 minutes or more. The VO2 steady-state is attained at a level higher then expected for a below 1st VT VO2/WR relationship. The slow component represents an additional cost due to progressive loss of muscle efficiency.
The high-to-severe intensity domain comprises all the work rates above the 2nd VT that determine a peak VO2 attainment with no steady state. In this intensity domain, no slow component is evident and VO2 rises close to a monoexponential pattern that is terminated at maximal VO2 (see Figure 2c). The severe-to-extreme intensity is a domain characterised by a very short tolerable duration; fatigue occurs before peak VO2 can be achieved.