How to Assess Benefits on Functional Capacity and Exercise Performance
An improvement in functional capacity is the most immediate and objective result of an effective ET programme. Despite the fact that functional capacity is governed by an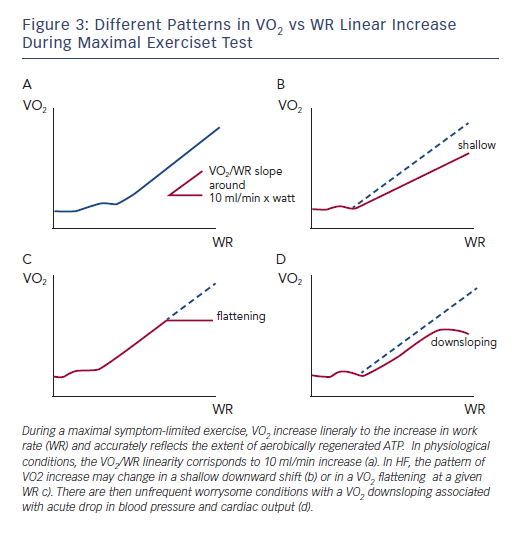
The question of how much ET may improve VO2 kinetics – rather than peak VO2 – is intriguing. Specifically, during maximal symptom-limited exercise, the VO2 increase is linearly related to the increase in WR and accurately reflects the extent of aerobically regenerated adenosine triphosphate (ATP). In physiological conditions, the VO2/WR linearity corresponds to a 10 ml/min increase per watt, irrespective of the load imposed and slightly changing according to exercise duration (see Figure 3a). This assumption, however, is not true in cardiovascular disorders such as HF and the pattern of VO2 increase may change in a shallow downward shift (see Figure 3b) or in a VO2 flattening at a given WR (see Figure 3c). Consequently, there are infrequent concerning conditions with a VO2 decrease associated with acute drop in blood pressure and cardiac output (see Figure 3d). Aside from this extreme condition, the other abnormal phenotypes may represent a very likely target of ET interventions worth of consideration even when changes in peak VO2 per se are not remarkable.
The other set of abnormalities that are typical of HF and may considerably benefit from ET interventions are those involving the inefficient ventilation (VE), which is an integral part of the abnormal response to exercise and represents a mainstay target of therapeutic interventions. Ventilation inefficiency is described by the slope of the rate of increase of VE vs carbon dioxide production (VCO2).16
VE/VCO2 slope is a clear, but underestimated, endpoint of ET. Studies that have addressed how exercise interventions may modulate exercise hyperpnoea have not been numerous, however, they have been consistent in showing a positive effect of ET (see Table 1).1,17–22 These studies have been performed with aerobic continuous ET of variable intensity and, on average, a reduction in the VE/VCO2 slope of around 10 % has been observed. Mechanisms implicated in this beneficial effects may be multifactorial, including a modulatory activity on chemoreflex sensistivity and an improved perfusion of lung microvessels.
Another important target of ET programmes is exercise oscillatory ventilation (EOV), a phenomenon charcaterised by a cyclic fluctuation of ventilation and expired gas kinetics, occurring in approximately 20–30 % of heart failure patients. The proposed aetiology includes a prolonged circulatory time with failure of cardiac output to adequately increase, causing delay in circulatory time and a demodulated chemoreflex sensitivity to blood gas tension.16
ET seems to be the most comprehensive intervention that is able to modulate at a multisystem level the pathogenetic mechanisms involved in this relevant ventilatory abnormality, by ‘resetting’ the central and peripheral control of VE23 and preventing the haemodynamic perturbations responsible for an increased circulatory time.24 In a trial by Zurek et al.21 the hypothesis was tested and confirmed: ET programmes may effectively impact EOV. Patients were optimally treated, 100 % were receiving renin–angiotensin system inhibitors and 90 % β-blockers, suggesting that EOV is a phenomenon that may not be responsive to standard HF therapy, requiring a targeted ad hoc approach, such as ET.
Future studies performed in large cohort of patients should aim to clarify how much ventilatory abnormalities may benefit from ET programmes, extending clinical endpoints to variables that, although pathophysiologically relevant, are still poorly analysed and considered.
Identification of ET Nonresponders
Some patients performing supervised ET do not show any improvement in exercise capacity and peak VO2 and represent a subset worthy of attention. Few studies have, however, addressed the clinical relevance of poor response to ET, though predicting nonresponders and how to successfully intervene by selecting appropriate and personalised intensity domain defined ET programmes would be of use.
In 155 HF patients undergoing an ET programme (aerobic continuous training at 1st VT workload), Tabet et al.25 identified a subgroup at higher risk that did not improve peak VO2 much and in need of a tight monitored. No mechanistic explanations were provided except for evidence at multivariate analysis of B-type natriuretic peptide level along peak VO2 as only independent predictive factors of outcome (p=0.01).
Interestingly, in a large group of HF patients Scmidt et al.26 provided the only available characterisation of ET responders identified as patients who did not improved peak VO2 by more than 5 % and work load by more than 10 %, or reduced VE/VCO2 slope by more than 5 %. Subjects who did not fulfil at least one of the above criteria were classified as non-responders. The best predictors of positive ET were HR recovery at 1 min, and peak HR and optimal thresholds separating responders from non-responders were at less than 30 bpm for HR reserve, less than 6 bpm for HR recovery and less than 101 bpm for peak HR.
In summary, it is intriguing to prospect that once more attention is posed on the nonresponder phenotype, ET should conceivably be switched to a personalised ET intensity domain that would yield to the most efficient and of ET-derived benefits across the wide spectrum of HF syndrome.