Conventional Risk Factors for SCD in HCM
The selection of patients who may benefit from ICD therapy for primary prevention purposes is more challengin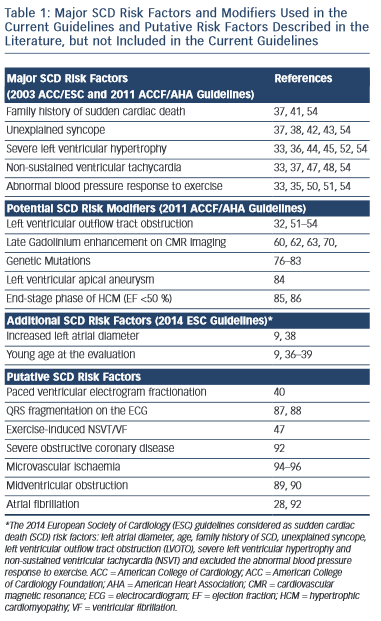 g. Several potential risk factors for SCD have been reported, however conventionally regarded major risk factors include unexplained syncope, family history of sudden cardiac death (FHSCD), severe left ventricular hypertrophy (LVH), non-sustained VT (NSVT) on the Holter-monitoring or during exercise and an abnormal blood pressure response to exercise (ABPRE) (see Table 1).19,28–32 Consistent with the clinical diversity of the disease, all of these risk factors have a relatively low positive predictive accuracy in the range of 20 %.29 Conversely, each factor has an excellent negative predictive accuracy therefore a patient who does not exhibit any of these risk factors is suitably deemed low risk.29,31 Nevertheless, up to 3 % of arrhythmogenic SCDs occur in patients who do not exhibit any of these risk factors.33,34
g. Several potential risk factors for SCD have been reported, however conventionally regarded major risk factors include unexplained syncope, family history of sudden cardiac death (FHSCD), severe left ventricular hypertrophy (LVH), non-sustained VT (NSVT) on the Holter-monitoring or during exercise and an abnormal blood pressure response to exercise (ABPRE) (see Table 1).19,28–32 Consistent with the clinical diversity of the disease, all of these risk factors have a relatively low positive predictive accuracy in the range of 20 %.29 Conversely, each factor has an excellent negative predictive accuracy therefore a patient who does not exhibit any of these risk factors is suitably deemed low risk.29,31 Nevertheless, up to 3 % of arrhythmogenic SCDs occur in patients who do not exhibit any of these risk factors.33,34
The significance of these risk factors is governed by age.32–39 In young patients, syncope, severe LVH and NSVT are particularly associated with an increased risk of SCD.30,35–39 In older patients who have survived more than 60 years, the risk of arrhythmogenic SCD is low despite the presence of the five conventional risk factors above.39
Invasive electrophysiological studies, such as programmed ventricular stimulation, have a poorer predictive accuracy than some of the risk factors mentioned above and is not indicated for risk stratification.30 Paced ventricular electrogram fractionation analysis has been reported to reveal a positive predictive accuracy in the range of 38 %.40 However, the invasive nature of the procedure in combination with the dynamic nature of the risk profile of SCD in HCM patients means that periodical assessment is impractical.
Family History of SCD
A FHSCD from HCM in first-degree relatives of an affected patient or the presence of one or more premature SCD in the family has always been considered to represent an important risk factor because it is recognised that SCD events often cluster in families.29 Patients receiving an ICD for primary prevention based on a family history of HCM-related SCD experience appropriate electrical discharges comparable to other patient subsets with high-risk markers.41
Unexp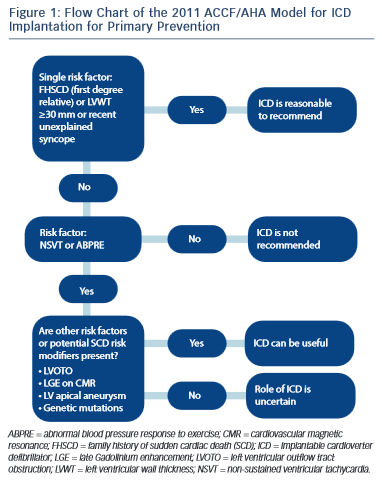 lained Syncope
lained Syncope
Determination of the possible cause of unwitnessed syncope is challenging in HCM because there are multiple potential causes that include vasovagal syncope, arrhythmogenic syncope, abnormal vascular responses or transient severe mechanical LVOTO.28 However, the clinical perception is that syncope is the only premonitory cardiac symptom that is associated with SCD.28,42,43 Patients with syncopal events that occur in close temporal proximity (6 months) to the initial evaluation, show a substantially higher risk of SCD than patients without syncope.38 Older patients with remote syncopal events do not show an increased risk.38
Severe Left Ventricular Hypertrophy
The severity and extent of LVH is associated with increased risk of SCD.30 Several studies have shown that a maximum wall thickness of ≥30 mm is associated with greatest risk of SCD.44–46 The ACCF/AHA guidelines state that the presence of extreme LVH alone is reasonable to recommend ICD29 (see Figure 1); however, extreme LVH is relative rare and the maximum wall thickness of a single segment may not adequately represent the true burden of hypertrophy.19 According to the 2003 ESC guidelines, the degree of maximum left ventricle (LV) wall thickness should be considered in the context of a multifactorial approach to risk stratification, rather than as an isolated risk factor.28,36 An excep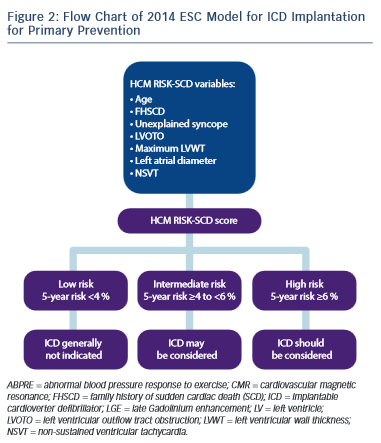 tion may be the development of severe LVH at a young age (<18 years).36
tion may be the development of severe LVH at a young age (<18 years).36
Non-sustained Ventricular Tachycardia
The presence of repetitive ventricular arrhythmias, at rest or effort- induced is frequently used as a marker of increased electrical instability of the myocardium in clinical practice.37,47 NSVT (defined as ≥3 consecutive beats with a heart rate of ≥120 bpm) is detected in approximately 20 % of HCM patients and is associated with a substantial increase in SCD risk in young patients aged ≤30 years old.37 A relationship between the frequency, duration and rate of NSVT episodes has not yet been clearly demonstrated.37 In clinical practice isolated brief runs of NSVT on random Holter-monitoring rarely trigger decisions for prophylactic ICD, whereas frequent and/or prolonged (>10 beats) bursts of NSVT identified over serial monitoring periods, intuitively carry greater weight as a risk factor.48 In one study of 104 HCM patients with an ICD the presence of NSVT was the most predictive risk factor for appropriate ICD discharge in the 78 patients of the primary prevention group.24
Abnormal Blood Pressure Response to Exercise
Approximately one-third of patients with HCM, have an ABPRE (defined as either the failure to increase by at least 20 mmHg or a drop of at least 20 mmHg during effort), which can be due to central and peripheral mechanisms.28,29,49 An ABPRE rarely represents the sole indication for a prophylactic ICD implant in clinical practice and is usually considered in association with other risk factors (see Figure 1).29,35 The 2014 ESC guidelines did not consider the ABPRE as a risk factor since it has not been independently associated with SCD in any multivariate survival analysis (see Figure 2).29,30,50,51