Specific Cases
Left Ventricular Aneurysm
Left ventricular apical aneurysm with regional scarring is considered as a potential risk factor for primary prevention and has recently been reported in a high-risk subset of HCM patients.84 Left ventricular apical aneurysm is rare (approximately in 2 % of HCM patients) and is b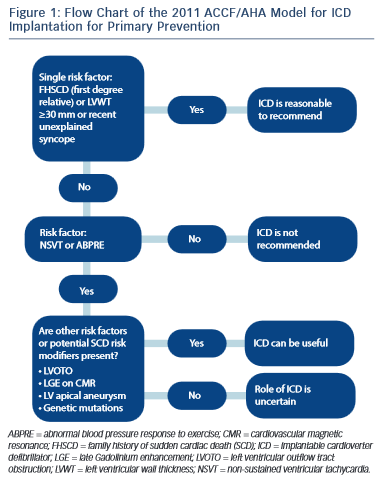 est characterised by CMR imaging. In one study of 28 patients, almost half of the patients with left ventricular apical aneurysm experienced adverse disease complications (event rate 10.5 %/year), including SCD, appropriate ICD discharges, non-fatal thromboembolic stroke and progressive heart failure and death.84
est characterised by CMR imaging. In one study of 28 patients, almost half of the patients with left ventricular apical aneurysm experienced adverse disease complications (event rate 10.5 %/year), including SCD, appropriate ICD discharges, non-fatal thromboembolic stroke and progressive heart failure and death.84
End-stage Phase of HCM
End-stage phase of HCM affects 3–8% of individuals and is characterised by progressive thinning of the myocardium with cavity enlargement and impaired systolic function.85,86 The complication is a result of extensive and transmural fibrosis and has a high incidence of SCD with an annual mortality rate exceeding 10 %.85,86 In such patients, prophylactic ICD implantation is a generally accepted clinical practice.29,85,86
2003 ACC/ESC Guidelines versus 2011 ACCF/AHA Guidelines
The main disagreement between the US and Europe guidleines is historically based on the number of risk factors required before consideration of an implantation of an ICD for primary prevention.28,29 Given the low positive predictive value of each of the conventional risk factors, the European approach has been to implant an ICD only in the presence of >1 risk factor.28 By contrast, the US approach recommends ICD implantation patients with FHSCD from HCM in a first-degree relative, LV wall thickness ≥30 mm or recent unexplained syncope as isolated risk factors whereas those patients with NSVT or an ABPRE require another risk factor or risk modifier (such as LVOTO, LGE on CMR imaging, LV apical aneurysm or a high-risk genetic mutation)29 (see Figure 1). This difference in approach is partially due to the conflicting results between American and European studies regarding the risk stratification.22,33 Previous American studies have reported that an important proportion of discharges occur in patients implanted with a prophylactic ICD with just one risk factor.22 The European concern is that if ICDs were inserted in all patients with one risk factor the incidence of device complications would surpass the potential benefits.33,34 Although there is no doubt about the value of an ICD in preventing SCD with appropriate discharge rates ranging from 2–3.6 %/year for primary prevention cases and 4.3–10.6 %/ year for secondary prevention cases, the inappropriate shock rate and implant complications range from 16–27 % and 12–18 %, respectively.22,23 A recent meta-analysis of 16 HCM cohorts reported inappropriate ICD interventions and complication of 4.8 %/year and 3.4 %/year, respectively.25
HCM Risk-SCD Model of the 2014 ESC Guidelines
A fundamental problem with the aforementioned risk stratification procedure is the assumption that the significance of all of the risk factors remains static throughout life. F urthermore, important parameters such as LVH or LVOTO, which are contiguous variables, are treated as binary factors (present or absent). The ESC HCM outcome investigators have recently recommended a 5-year risk calculator derived from a model involving a large retrospective longitudinal multicentre experience from 3,675 patients.9,30 Eight clinical parameters were included as pre- specified predictors that were independently associated with SCD in at least one published study of multivariate survival analysis. Of the eight parameters, seven were associated with SCD or an appropriate ICD shock at the 15 % significance level and these were: age, FHSCD, maximal LV wall thickness, left atrial diameter, maximal LVOTO, NSVT and unexplained syncope (see Figure 2).
urthermore, important parameters such as LVH or LVOTO, which are contiguous variables, are treated as binary factors (present or absent). The ESC HCM outcome investigators have recently recommended a 5-year risk calculator derived from a model involving a large retrospective longitudinal multicentre experience from 3,675 patients.9,30 Eight clinical parameters were included as pre- specified predictors that were independently associated with SCD in at least one published study of multivariate survival analysis. Of the eight parameters, seven were associated with SCD or an appropriate ICD shock at the 15 % significance level and these were: age, FHSCD, maximal LV wall thickness, left atrial diameter, maximal LVOTO, NSVT and unexplained syncope (see Figure 2).
The incorporation of these parameters into the model equation is used to estimate the 5-year risk of SCD for any particular patient. The cut-off level of ≥6 % SCD risk in 5 years is recommended for considering an ICD implant for primary prevention. Individuals with a risk score of <4 % are considered as low risk, whereas those with a risk score of 4–6 % of SCD characterise an intermediate-risk group where ICD may be considered (see Figure 2).
The results of this study indicate that the use of this model is superior to prior conventional methods for detecting high-risk individuals previously considered at low or intermediate risk. The model also scores highly for correctly identifying individuals at high risk of SCD.30
The new 2014 ESC risk stratification model is limited to some extent in that it was not validated in paediatric patients (<16 years), in patients with syndromic LVH or in a large population of non-Caucasian individuals. Furthermore the effect of latent LVOTO or the effect of LVOTO reduction by alcohol ablation or myectomy was not tested and very few patients had extreme LVH ≥35 mm.30
Other Potential Risk Factors and Arbitrators not Included in the Current Guidelines
A number of electrical, structural and functional markers that can be assessed using simple investigations have been proposed for risk stratification. The fragmentation of the QRS on the ECG has been postulated to predict ventricular arrhythmic events.87,88 A study in 167 patients with a mean follow-up of 6.3 years, fragmentation of the QRS was a strong independent predictor for major arrhythmic events including SCD.87
There are reports that HCM associated with midventricular obstruction (with pressure gradient ≥30 mmHg) may be an independent predictor of adverse outcomes, especially the combined endpoint of SCD and potentially lethal arrhythmic events.89,90 Conversely, apical HCM has been associated with a benign prognosis.91
Myocardial ischaemia that may be caused by small vessel disease or concomitant severe epicardial coronary artery disease has also been considered as possible risk factor.28,92,93 In one study of 433 HCM patients, 27 % had severe epicardial CAD and this was a significant predictor for cardiac death and SCD.92 Assessment of coronary microvascular dysfunction is challenging and stress perfusion CMR imaging could have a future role in risk stratification.94–96 Exercise capacity has also been proposed to help risk stratification in different studies.97–99 It has been demonstrated that peak VO2 is associated with an increased risk of major events during short-term follow-up.99