Primary Prevention
Current evidence supports the use of statins in individuals without vascular disease at higher ASCVD risk for the primary prevention of future cardiovascular events.7–9 In the most recent meta-analysis which included ~60,000 individuals by Taylor et al., authors concluded statin therapy is associated with a 14 % reduction in all-cause mortality and a 35 % reduction in combined fatal and non-fatal cardiovascular disease, coronary heart disease and stroke.8 The 2013 ACC/AHA cholesterol guidelines recommend use of high-intensity or moderate-intensity statins (see Table 1) in individuals with 10 year ASCVD risk of 7.5 % or greater using the pooled cohort equation (PCE). In 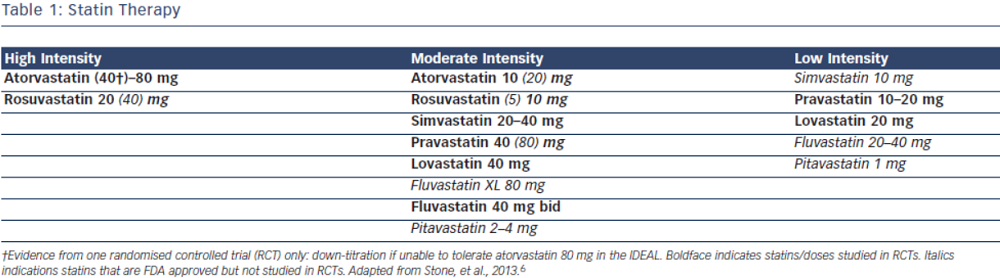 individuals with a PCE score of 5–7.5 % consideration should be given to treatment with moderate dose statin based on the presence of other risk factors such as family history, LDL-C level, inflammatory markers, coronary calcium score, ankle-brachial index and lifetime risk.6 Decision to choose between high-intensity and moderate-intensity statin can be taken by the individual provider, weighing the risk/benefit ratio of statin side effects. Elderly patients and those with a history of myalgia or risk factors for statin intolerance should be started on moderate-intensity statins.10–13 However, patients with LDL>190 should be on high intensity statins.6 ESC/EAS guidelines recommend treatment with statin for patients in the high-risk group and targeting goal LDL-C levels <70 mg/dL (2.5 mmol/L) for high-risk groups based on SCORE chart or those with LDL-C levels >190 mg/dL (4.9 mmol/L).5
individuals with a PCE score of 5–7.5 % consideration should be given to treatment with moderate dose statin based on the presence of other risk factors such as family history, LDL-C level, inflammatory markers, coronary calcium score, ankle-brachial index and lifetime risk.6 Decision to choose between high-intensity and moderate-intensity statin can be taken by the individual provider, weighing the risk/benefit ratio of statin side effects. Elderly patients and those with a history of myalgia or risk factors for statin intolerance should be started on moderate-intensity statins.10–13 However, patients with LDL>190 should be on high intensity statins.6 ESC/EAS guidelines recommend treatment with statin for patients in the high-risk group and targeting goal LDL-C levels <70 mg/dL (2.5 mmol/L) for high-risk groups based on SCORE chart or those with LDL-C levels >190 mg/dL (4.9 mmol/L).5
Atherosclerotic Cardiovascular Disease
The 2013 ACC/AHA guidelines recommend use of high-intensity statins in individuals with known ASCVD, specifically atorvastatin 80 mg or rosuvastatin 20–40 mg.6 In the Cholesterol Treatment Trialist (CTT) Collaboration meta-analysis including over 170,000 individuals, the authors concluded that more intensive statin therapy and lower LDL-C levels resulted in further reductions in major cardiovascular events. High-intensity statin therapy demonstrated 15 % reduction in major cardiovascular events as compared to low intensity statins. Overall, authors found that all-cause mortality was reduced by 10 % per 1.0 mmol/L reduction in LDL-C.2 In patients with ASCVD the evidence overwhelmingly supports treatment with high dose statins such as atorvastatin 80 mg or rosuvastatin 20–40 mg daily regardless of baseline LDL-C levels. The ESC/EAS guidelines approach ASCVD as high risk and recommend targeting LDL-C levels <70 mg/dL (<1.8 mmol/L) or at least a 50 % reduction in LDL-C. These guidelines also recommend combination therapy if target cannot be reached with statin only.5
Chronic Kidney Disease
Currently under the new ACC/AHA 2013 cholesterol guidelines, chronic kidney disease (CKD) is not classified as a coronary heart disease (CHD) equivalent and does not factor into the risk calculator.6 This differs from ESC/EAS guidelines which place CKD patients into the high risk category.5 Studies have shown increased cardiovascular events and mortality in with patients with decreased estimated glomerular filtration rate (eGFR) and albuminuria.14,15 Independent of lipid effects, a meta-analysis, which included 6,452 CKD patients randomised to statin versus placebo, showed renoprotective effects of statins. Statin therapy was associated with significant reductions in urinary protein excretion (0.77 g/24 h) and creatinine (0.65 mg/ dl), but improvement in creatinine levels was only associated with long-term statin use (>3 years). Significant increase in eGFR was also found between 1–3 years on statin therapy, but this improvement in renal function did not persist beyond three years.16 The Study of Heart and Renal Protection (SHARP) trial directly assessed the cardiovascular benefit of statins in patients with CKD. This study randomised 9,438 adults to the combination simvastatin 20 mg/ ezetimibe 10 mg versus placebo and found a 17 % reduction in cardiovascular events in those allocated to statin/ezetimibe.17 This benefit was not completely from statins, as previous studies have demonstrated the efficacy of ezetimibe added to statins. A recent meta-analysis comparing combination therapy versus statin monotherapy included 11 studies on ezetimibe and concluded an additional 18 % reduction of LDL-C with the addition of ezetimibe.18 These findings are reflected in the new guidelines from the Kidney Disease: Improving Global Outcomes (KDIGO) group, which recommends statin/ezetimibe combination therapy for adults >50 years old with eGFR<60 ml/min/1.73 m2 who are not treated with chronic dialysis or kidney transplantation. In adults aged 18–49 with CKD, consideration should be given to statins if they also have risk factors such as known CHD, diabetes mellitus, prior ischaemic stroke or elevated cardiovascular risk score.19 Atorvastatin is recommended in CKD because of its favourable pharmacokinetics and minimal renal excretion negating need for dose adjustment. Rosuvastatin can also be used safely in patients with advanced CKD (GFR<30 ml/ min/1.73 m2), but should be started at 5 mg daily and titrated up to maximum of 10 mg daily if needed.20
Patients on chronic dialysis have been directly studied in randomised controlled trials and appear not to benefit from statin therapy. In the 4D study, 1,255 patients with diabetes mellitus receiving maintenance haemodialysis were randomised to atorvastatin 20 mg or placebo with no difference in cardiovascular death, stroke or non-fatal myocardial infarction (MI) in the two groups after a median follow-up of four years.21 A Study to Evaluate the Use of Rosuvastatin in Subjects on Regular Hemodialysis: An Assessment of Survival and Cardiovascular Events (AURORA) randomised 2,776 patients on maintenance haemodialysis to rosuvastatin 20 mg versus placebo and again found no benefit in the statin group.22 Therefore, statins should not be initiated in patients on maintenance haemodialysis.
Diabetes Mellitus
Diabetes Mellitus (DM) is associated with increased risk of cardiovascular diseases23,24 and early onset is considered a CHD risk equivalent.25 Current guidelines recommend treatment with at least moderate intensity statin for all adults >40 years old and high intensity statin for those with a 10 year risk score >7.5 %.6 ESC/EAS guidelines recommend statins for patients with diabetes only when they develop evidence of end organ damage.5