The Electrocardiogram – a Key to the Diagnosis of the Brugada Syndrome
The standard 12-lead ECG (with some additional modifications, as explained below) is crucial for the diagnosis and likely also for determining the prognosis (i.e. the level of arrhythmic risk) in the BrS. The diagnostic hallmark of syndrome is the so-called “coved” or “type 1 Brugada ECG pattern” characterised by J-point elevation with slowly descending or concave ST segment elevation merging into a negative or reaching the isoelectric line symmetric T wave7,34 (see Figure 1A). The type 1 Brugada ECG pattern is observed most frequently in leads V1 and V2, much less frequently in lead V3.35 When type 1 Brugada ECG pattern is observed in lead V3 it is always accompanied by the same ECG pattern in at least one more right precordial lead (unpublished observations).
In patients investigated for the BrS, leads V1 and V2 should always be recorded both from the 4th intercostal (i.c.) space as well as from the 3rd and 2nd i.c. space, because the “high” positions increase the sensitivity of leads V1 and V2 for detecting type 1 pattern without loss of specificity36 (see Figure 2). This has been noted already in 1960,37 long before the discovery of the Brugada syndrome. Since the exact anatomic relation between RV and the thoracic cage is individually specific and any of the three i.c. spaces could be closest to the RVOT, it is best to record simultaneously leads V1 and V2 in the 4th, 3rd and 2nd i.c. space. One small study with cardiovascular magnetic resonance imaging found that the maximum RVOT area was most frequently in the 3rd followed by the 4th and 2nd i.c. space.38 In our experience, when type 1 Brugada pattern is observed in the 4th i.c. space it is always also observed in the 3rd or 2nd i.c. space whereas the converse is not the case (unpublished observations). Positioning lead V3 one or two i.c. spaces higher also increases its sensitivity to detect type 1 pattern (unpublished data) (see Figure 2). Bipolar precordial leads between the V2 electrode (positive pole) and V4 or V5 electrodes (negative pole) which can be computed from the standard unipolar leads V2, V4 and V5 seem to be more sensitive and equally specific compared to the unipolar lead V2 for detecting the diagnostic type 1 Brugada ECG pattern.39 Type 1 Brugada ECG pattern sometimes also can be observed in the inferior40,41,42,43 or lateral44,45 leads (the so-called “atypical” BrS).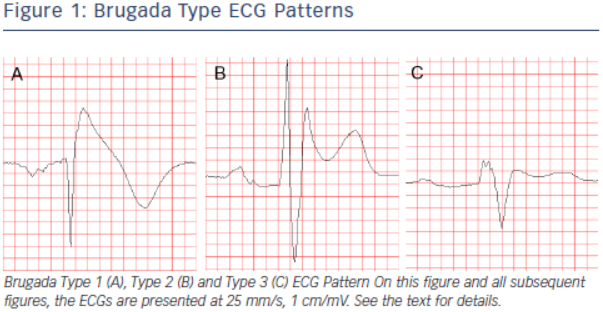
Another ECG pattern of J point and ST segment elevation with a positive T wave in the right precordial leads, the so-called “saddleback” pattern, is considered suspicious but not diagnostic of BrS, unless converted into type 1 pattern following administration of Na+ channel blocking agents. Traditionally the “saddle back” patterns are further divided into “type 2” and “type 3” Brugada ECG pattern depending on the level of J point and ST segment elevation2 (see Figure 1B,C). A recently published expert Consensus Report on the ECG characteristics of the BrS proposed “type 2” and “type 3” patterns to be unified into one “saddle-back” Brugada pattern because, according to the authors’ opinion, the small morphological differences between the two patterns had no diagnostic or prognostic significance.34 In the latest HRS/EHRA/APHRS Expert Consensus Statement on the Diagnosis and Management of Patients with Inherited Primary Arrhythmia Syndromes published in December 2013,7 however, type 2 and type 3 Brugada ECG patterns are still mentioned separately.
Up to 40 % of patients with the BrS present with normal or nondiagnostic resting ECG.46 In these patients, the diagnostic “coved” ECG pattern can be elicited by i.v. administration of sodium channel blocker (ajmaline, procainamide, flecainide).47,48 Currently the BrS is definitely diagnosed when type 1 pattern is observed in at least one of leads V1 and V2 recorded from the 4th, 3rd or 2nd i.c. space either spontaneously or following administration of Na+channel.7 The presence of gene mutations is not considered essential for the diagnosis.2,7
It is important to distinguish between type 2 Brugada ECG pattern and the r’or R’-pattern (incomplete right bundle branch block (iRBBB) pattern) in leads V1 and V2 (especially when recorded from the 3rd or 2nd i.c. space) which can be observed in healthy subjects (frequently in athletes49). It has been reported that a broader angle between the ascending and descending limb of the r’/R’-wave50 or a broader base of the triangle formed by the two limbs of the r’/R’-wave measured at 5 mm from the highest point51,52 can reliably distinguish type 2 Brugada ECG pattern from IRBBB pattern. The classical diagnostic type 1 Brugada ECG pattern needs to be distinguished from similar “Brugadalike” patterns caused by RBBB, septal hypertrophy, arrhythmogenic right ventricular cardiomyopathy (ARVC), pectus excavatum and other conditions, and also from the transient appearance of typical Brugada pattern in the cause of various acute processes such as acute ischaemia, Prinsmetal angina, pulmonary embolism, pericarditis, metabolic disorders, various medications and others (the so-called “Brugada phenocopies”,53 see www.brugadaphenocopy.com). The ECG characteristics of the BrS and the methods to distinguish them from other conditions presenting with similar ECG changes are reviewed in great detail in the above mentioned ECG Consensus Report.34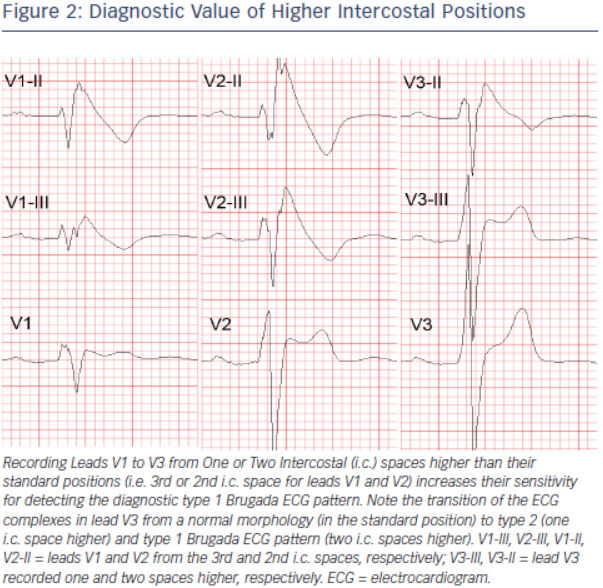
ECG acquisition with inappropriate high-pass filtering (e.g. non-linear phase high-pass filter of 0.5 Hz instead of the recommended 0.05 Hz)54 can cause considerable ST segment distortion and even mimic type 1 or 2 Brugada pattern.34,55,56
The ECG in BrS characteristically shows considerable dynamic variability; it can be completely normal at one time and demonstrate diagnostic type 1 pattern at another. Vagal influences (slow heart rate, post-prandial state, nighttime) tend to augment the J point and ST segment elevation and the type 1 pattern,57 whereas exercise and catecholamine infusion tend to have the opposite effect (however, in some BrS patients the ST segment elevation might become more prominent during exercise).58 Autonomic influences play important role also in the genesis of malignant arrhythmias because most of the arrhythmic events in BrS occur at night, two long RR intervals often precede episodes of VT/VF,59 whereas catecholamine infusion is used as a first line treatment of such episodes.60 Patients with BrS have increased incidence (10–53 %) of atrial fibrillation (AF).61,62 Additional ECG findings which support the diagnosis of the BrS in asymptomatic patients with spontaneous or induced by Na-channel blockers type 1 pattern include the presence of atrial fibrillation, atrio-ventricular or intraventricular conduction abnormalities (first degree A-V block, fragmented and/or prolonged QRS, abnormal signal-averaged ECG (SAECG), left axis deviation of the QRS complex, prolonged HV interval), ventricular ectopic beats with left bundle branch block (LBBB) morphology and short (<200 ms) ventricular effective refractory period.7