ECG-derived Parameters for Risk Assessment
Similarly to other diseases with intraventricular conduction abnormalities such as IHD and cardiomyopathies,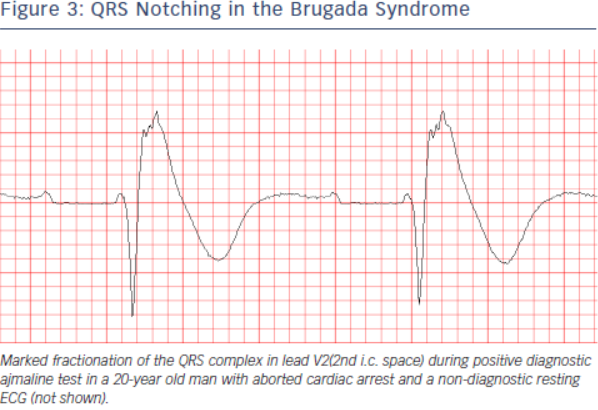 the presence of notched or fragmented QRS,31,83 (see Figure 3) has been consistently demonstrated to indicate increased arrhythmic risk independently of other clinical and ECG variables (HR 4.9, 95 % CI 1.6-15.4 in the PRogrammed ELectrical stimUlation preDictive valuE (PERLUDE) study).85
the presence of notched or fragmented QRS,31,83 (see Figure 3) has been consistently demonstrated to indicate increased arrhythmic risk independently of other clinical and ECG variables (HR 4.9, 95 % CI 1.6-15.4 in the PRogrammed ELectrical stimUlation preDictive valuE (PERLUDE) study).85
 However, currently the presence of notching/fractionation is assessed only visually using arbitrary descriptive criteria (e.g. number of QRS peaks). The presence of late potentials on the signal-averaged ECG (SAECG) is another marker of intraventricular conduction disturbances which also indicates increased arrhythmic risk in BrS30 independently of QRS fractionation. The standard time-domain SAECG, however, cannot detect conduction abnormalities within the QRS complex, has uncertain value in patients with bundle branch block, and uses only a single-lead ECG complex which is derived from the XYZ orthogonal leads and does not contain any regional information.
However, currently the presence of notching/fractionation is assessed only visually using arbitrary descriptive criteria (e.g. number of QRS peaks). The presence of late potentials on the signal-averaged ECG (SAECG) is another marker of intraventricular conduction disturbances which also indicates increased arrhythmic risk in BrS30 independently of QRS fractionation. The standard time-domain SAECG, however, cannot detect conduction abnormalities within the QRS complex, has uncertain value in patients with bundle branch block, and uses only a single-lead ECG complex which is derived from the XYZ orthogonal leads and does not contain any regional information.
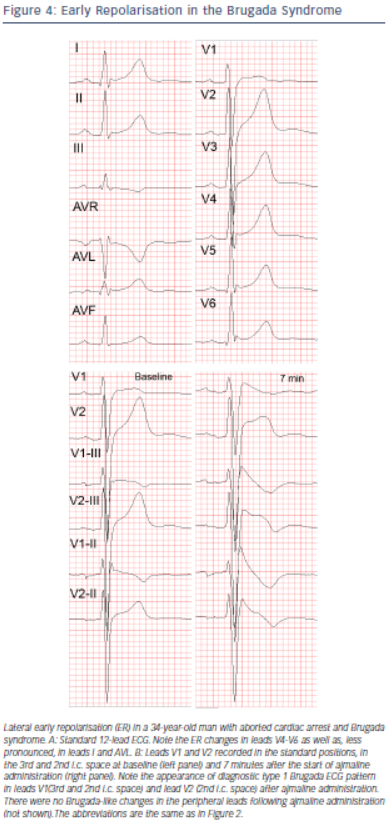
Among asymptomatic BrS patients, those with Brugada ECG pattern in the infero-lateral leads in addition to the right precordial leads,88 (increased “spatial Brugada burden”) were recently demonstrated to have several times higher risk of VF compared to those with Brugada type 1 changes only in the right precordial leads.89 On the other hand, the number of right precordial leads displaying type 1 pattern and the degree of J-point or ST-segment elevation do not seem to correlate with the arrhythmic risk.35,36 The “high” (3rd or 2nd i.c. space) positions of leads V1 and V2 are diagnostically more sensitive than their standard positions in the 4th i.c. space90,91,92 but prognostically their value is the same.93
Infero-lateral early repolarisation (ER) (see Figure 4) is not only more common (up to 15 %94) in BrS patients,70,94,95 but also carries up to 4-fold increased risk of spontaneous VF67,70 and even higher risk if the ER has “malignant” morphology,96 i.e. is associated with horizontal/descending (as opposed to rapidly ascending) ST segment after the J point.68,75 The combination of infero-lateral ER and fractionated QRS complex seems to indicate indicate a particularly high arrhythmic risk.97
Currently there are only limited data suggesting that other ECG parameters may indicate increased arrhythmic risk. These parameters include changes in repolarisation dynamics (QT/RR and Tpeak-Tend/RR intervals relations),98 deep negative T wave in lead V1,99< QTc interval more than 460 ms in lead V2 and prolonged Tpeak-Tend interval,100 dynamic alterations in the amplitude of the ST elevation,101 prolonged PR-interval,93 presence of atrial arrhythmias,60,61,102 and augmentation of the ST segment elevation during the early recovery phase of exercise test.103