Risk Stratification and the Prediction of Outcome Using Echocardiography
Asymptomatic Aortic Stenosis with Normal Left Ventricular Ejection Fraction
Peak Aortic Stenosis Velocity and the Rate of Haemodynamic Progression
VAS is the strongest predictor of clinical outcome, even in the subgroup with severe AS.1,2,42–45 For asymptomatic AS patients with VAS<3m/s, 3–4 m/s and >4 m/s, approximately 15 %, 35 % and 75 % of patients, respectively, will develop symptoms requiring AVR within three years.1–3,42,45 VAS>5.5 m/s is associated with a poor three year event-free survival of only 11 %,44 and the European Society of Cardiology (ESC) and American Heart Association (AHA)/ American College of Cardiology (ACC) valve guidelines consider AVR reasonable in these asymptomatic patients if the surgical risk is low (IIa recommendation).9,10 AVA also 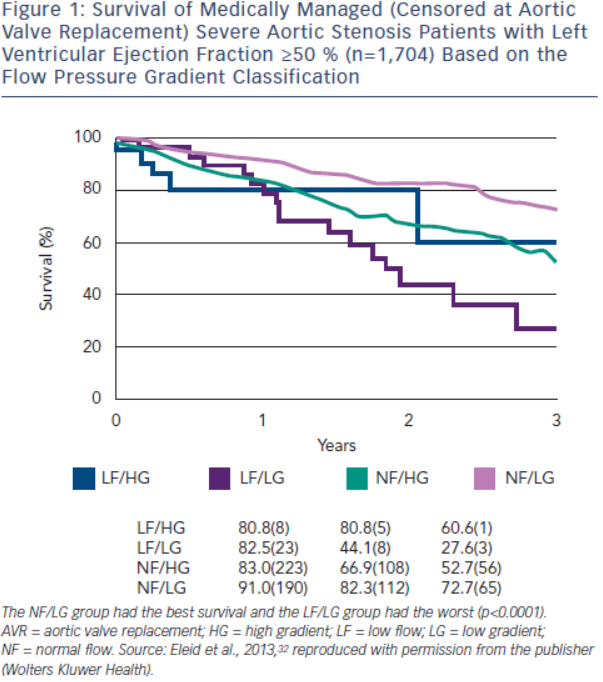 predicts event-free survival, although the relationship is not as robust as VAS.1,42,43,46 This may relate in part to an inherent bias by which clinicians may be more likely to refer patients with a higher VAS or MG for AVR. Rapid haemodynamic progression, defined as an increase in VAS≥0.3 m/s/yr, identifies patients at increased risk for clinical events.1,3,45 Severe AS patients with rapid haemodynamic progression have an event rate as high as 80 % in two years,3 and according to the ESC and AHA/ACC valve guidelines, AVR may be considered in an asymptomatic patient at low surgical risk (IIa and IIb recommendation, respectively).9,10
predicts event-free survival, although the relationship is not as robust as VAS.1,42,43,46 This may relate in part to an inherent bias by which clinicians may be more likely to refer patients with a higher VAS or MG for AVR. Rapid haemodynamic progression, defined as an increase in VAS≥0.3 m/s/yr, identifies patients at increased risk for clinical events.1,3,45 Severe AS patients with rapid haemodynamic progression have an event rate as high as 80 % in two years,3 and according to the ESC and AHA/ACC valve guidelines, AVR may be considered in an asymptomatic patient at low surgical risk (IIa and IIb recommendation, respectively).9,10
Valve Calcification
Valve calcification is best evaluated clinically using MDCT. However, valve calcification assessed by echocardiography is a strong predictor of haemodynamic and clinical progression across the spectrum of disease severity, and independent of the haemodynamic severity.3,45 Calcification can be graded as none, mild (isolated small spots), moderate (multiple bigger spots) and severe (extensive thickening/calcification of all cusps). Severe AS patients with moderate or severe valve calcification have an event rate of 80 % at four years, but only 25 % with no or mild calcification.3
Flow Pressure Gradient Classification
Patients with AVA≤1.0 cm2 and a normal LVEF can be classified into four subtypes based on the presence of:
Most patients (52–73 %) have the NF/HG pattern, in which MG and AVA are concordant for severe AS and SVi is normal.30,32,36,37 The NF/ LG pattern is present in 15–31 %, and encompasses patients with inherent inconsistencies in the cut-points for severe AS, small body size and prolonged ejection times in which SVi is normal but transvalvular flow rate may be reduced. The LF/HG pattern is observed in 3–13 %, and includes patients with concordant indices but intrinsic left ventricular dysfunction despite a normal LVEF. The LF/LG pattern is present in 3–19 % of patients, a group characterised by discordant haemodynamic indices and a low flow state.
The flow pressure gradient classification provides important prognostic information for severe AS patients with a normal LVEF. The NF/LG pattern has the highest event-free survival, while the LF/LG pattern has the worst outcome.32,34,37,47 The NF/HG and LF/HG patterns have intermediate survival. In Eleid et al.,32 survival with medical management (censored at AVR) at two years was 82 % in NF/LG patients, 81 % in LF/HG patients, 67 % in NF/HG patients and 44 % in LF/LG patients (p<0.0001) (see Figure 1). AVR conferred a strong survival benefit in LF/LG and NF/HG patients, but no benefit in NF/LG patients. However, other investigators have observed a survival benefit of AVR in both symptomatic LF/LG and NF/LG patients.48–51 SVi appears to be an important marker of prognosis and has a graded association with mortality in severe low gradient AS patients with preserved LVEF.52,53
Left Ventricular Function
Only a minority of severe AS patients present with a reduced LVEF and the prognosis is poor without AVR.9,54 However, a large proportion of severe AS patients with normal LVEF have intrinsic systolic dysfunction with abnormal global longitudinal strain on speckle tracking imaging.55–57 Patients with moderate or severe AS and global longitudinal strain ≤15 % have a poor two-year event-free survival of ≈30 %, as compared with 65 % if >15 %.56,57 There are no data to justify AVR in asymptomatic patients with impaired longitudinal strain, although close follow-up is likely warranted.
Valvular Arterial Impedance
Valvular arterial impedance (Zva) provides a measure of global LV load due to the valve stenosis and VAScular afterload. Zva is calculated as (SBP+MG)/SVi, 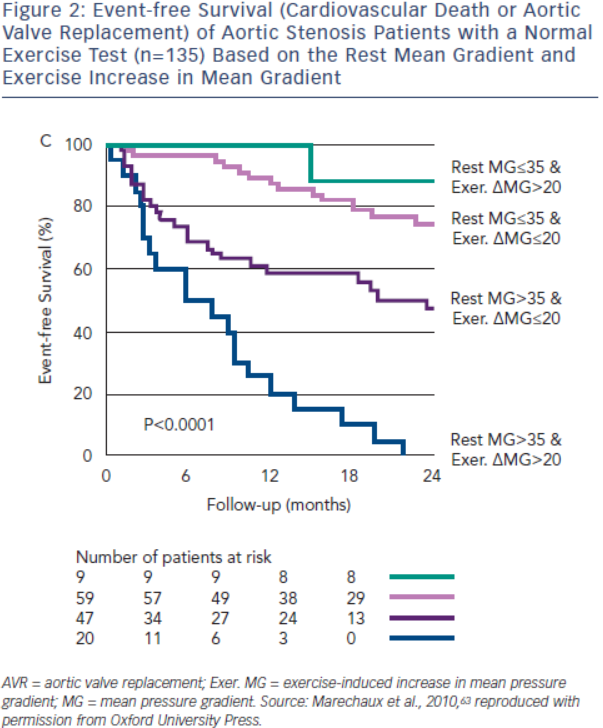 where SBP is the systolic blood pressure.58 In asymptomatic patients with moderate or severe AS, Zva>4.5–5.0 mmHg/ml/m2 predicts reduced event-free survival and a 2.8-fold increased risk of death;56,58 however, Zva does not identify the relative contributions of the valve and VASculature that is necessary to guide management (i.e. AVR versus blood pressure [BP] control).
where SBP is the systolic blood pressure.58 In asymptomatic patients with moderate or severe AS, Zva>4.5–5.0 mmHg/ml/m2 predicts reduced event-free survival and a 2.8-fold increased risk of death;56,58 however, Zva does not identify the relative contributions of the valve and VASculature that is necessary to guide management (i.e. AVR versus blood pressure [BP] control).
Exercise Echocardiography
More than 50 % of patients with asymptomatic severe AS develop symptoms within three years, and the subsequent prognosis is poor without timely AVR.1–3,8 Exercise testing can unmask symptoms in as many as one third of patients and a positive exercise test predicts the need for AVR or death.59–61 The ESC and AHA/ACC valve guidelines consider AVR indicated in asymptomatic severe AS patients with symptoms on exercise testing (Class I recommendation) or a drop in BP (IIa recommendation).9,10
Exercise echocardiography may provide additional prognostic information beyond the exercise test. An exercise increase in MG>18–20 mmHg potentially identifies severe AS patients at increased risk for symptoms, AVR or death, even with a normal exercise test (see Figure 2).62,63 The adverse prognosis of patients with greater increases in MG likely reflects a more severely stenotic or non-compliant valve with minimal opening reserve. In the ESC guidelines, AVR may be considered in these patients if the surgical risk is low (IIb recommendation).10 Failure of LVEF to increase with exercise is also associated with an abnormal exercise test and reduced event-free survival (event-free survival <40 % at two years).64 Although not specifically addressed in either valve guidelines, these patients should at a minimum be observed closely for surgical indications. Resting and exercise changes in global longitudinal strain are associated with an abnormal stress test and reduced event-free survival; however, their incremental prognostic value requires further study.55,65
Pulmonary hypertension is associated with poor outcomes and higher complication rates with valve intervention.66,67 The prevalence of pulmonary hypertension at rest in asymptomatic AS patients is low; however, exercise-induced pulmonary hypertension may develop in >50 % of severe AS patients.68 Pulmonary systolic pressure >60 mmHg with exercise is associated with a twofold increased risk of cardiac events and a reduced cardiac event-free survival at three years (22 ± 7 versus 55 ± 9 %; p=0.014), independent of the change in MG with exercise.68 Exercise pulmonary hypertension appears to unmask a severe impairment of diastolic function. Close follow-up of these patients is likely warranted.