Non-alcoholic Fatty Liver or Non-alcoholic Steatohepatitis?
The question whether the role of NAFLD in the development of CVD is confined to NASH or is already present in NAFL is important. Only about 5–10 % of 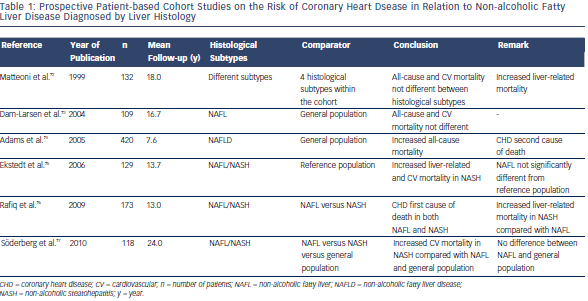 NAFLD patients have NASH,2 so if the risk were to be confined to NASH, this would substantially reduce the CVD burden attributable to NAFLD. This might be in contrast with the current data on the impact of NAFLD on CVD, which does not seem to fit with the relatively small number of NASH patients within the NAFLD group. The answer to this question has potential implications for the management of NAFLD patients. Indeed, if not only NASH but also NAFL were to be associated with an increased risk of CVD, one might argue that NAFLD should be treated regardless of the presence of NASH. NAFL would then turn out not to be a benign condition, as it still is generally regarded nowadays,2,11,12,15 and guidelines for the treatment of NAFLD might have to consider treating NAFL, with prevention of CVD as treatment indication.
NAFLD patients have NASH,2 so if the risk were to be confined to NASH, this would substantially reduce the CVD burden attributable to NAFLD. This might be in contrast with the current data on the impact of NAFLD on CVD, which does not seem to fit with the relatively small number of NASH patients within the NAFLD group. The answer to this question has potential implications for the management of NAFLD patients. Indeed, if not only NASH but also NAFL were to be associated with an increased risk of CVD, one might argue that NAFLD should be treated regardless of the presence of NASH. NAFL would then turn out not to be a benign condition, as it still is generally regarded nowadays,2,11,12,15 and guidelines for the treatment of NAFLD might have to consider treating NAFL, with prevention of CVD as treatment indication.
However, the question remains largely unanswered. The main reason is that most of the data come from studies where NAFLD is diagnosed based on ultrasound or on liver biochemistry or both.5,6 In these studies no distinction is made between NAFL and NASH. This distinction still requires a biopsy.13 Series including histology have smaller patient numbers and patients are usually more selected, leading to a potential overrepresentation of more severe liver disease compared with the general population. Furthermore, most of these studies have rather short mean follow-up times. The methodological limitations of these studies hamper the general applicability of their results.
Nevertheless, several data give an indication that the risk is confined to NASH, or is at least higher in NASH patients compared with NAFL. A first indication comes from the studies using liver biochemistry to diagnose NASH. Although it has been well-established that transaminases and gamma-glutamyl transpeptidase (GGT) are not perfectly correlated to the severity of the liver lesions, and that transaminases can be normal in patients with NASH79 as well as NASH can be present in patients with normal transaminases,86 overall liver enzymes are higher in NASH versus NAFL patients.79,87 Moreover, several scoring systems for NASH and NASH-related fibrosis include transaminases or GGT.79;88–91
A second indication comes from the studies that did include a liver biopsy and hence a histological classification of NAFLD. These studies are summarised in Table 1. Matteoni et al. only found differences in liver-related mortality but not in all-cause or other cause mortality according to histological subtype of NAFLD.92 Dam-Larsen et al. did not find differences in mortality comparing histologically proven patients with NAFL compared to the general population.93 However, more recent studies consistently show CVD being more prevalent in NAFLD patients, three out of four confining this risk to patients with NASH.94–97 In the study examining prothrombotic factors, we also found an increase mainly in PAI-1 in association with more severe histological lesions, mainly confining the elevations in PAI-1 to patients with NASH.74 Studies on levels of angiogenic factors in patients with NAFLD also showed the most pronounced changes in patients with NASH.69
Although these most recent data suggest that the risk is mainly associated with NASH, or is at least more pronounced in patients with NASH compared with NAFLD, further methodologically stringent studies with long-term follow-up are needed to solve this question.