Primary Percutaneous Coronary Intervention – Procedural Aspects and Issues
Radial Over Femoral Access In Experienced Operators (Class IIa, Level of Evidence B)
The role of radial access has been investigated for 20 years5 but in STEMI patients this topic has been especially highlighted. 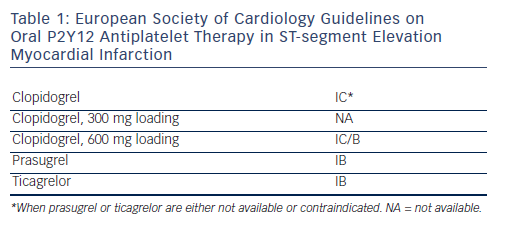 The Radial Versus Femoral Access for Coronary Intervention (RIVAL) STEMI subanalysis6,7 (1,958 patients) and Radial Versus Femoral Investigation in ST Elevation Acute Coronary Syndrome (RIFLE-STEACS)8 trial (1,001 patients) demonstrated a significant mortality benefit in a large cohort of STEMI patients treated with primary PCI via transradial approach (TRA) (44 % reduction in all-cause death in RIVAL STEMI and 60 % in cardiac death in RIFLE-STEACS). These findings were supported by two large meta-analyses published recently by De Luca et al.9 and Karrowni et al.10 In the contrary, no survival benefit was found in the ST Elevation Myocardial Infarction Treated by RADIAL or Femoral Approach in a Multicenter Randomized Clinical Trial (STEMIRADIAL) in 707 patients.11 Although the direct association between the radial access and mortality may still be doubtful, the significantly lower risk of vascular and bleeding complications should promote the TRA as the preferred access site for most operators.12 Proper training and enough experience are necessary to achieve the optimal results that should receive the strongest level of evidence A in the upcoming guidelines.
The Radial Versus Femoral Access for Coronary Intervention (RIVAL) STEMI subanalysis6,7 (1,958 patients) and Radial Versus Femoral Investigation in ST Elevation Acute Coronary Syndrome (RIFLE-STEACS)8 trial (1,001 patients) demonstrated a significant mortality benefit in a large cohort of STEMI patients treated with primary PCI via transradial approach (TRA) (44 % reduction in all-cause death in RIVAL STEMI and 60 % in cardiac death in RIFLE-STEACS). These findings were supported by two large meta-analyses published recently by De Luca et al.9 and Karrowni et al.10 In the contrary, no survival benefit was found in the ST Elevation Myocardial Infarction Treated by RADIAL or Femoral Approach in a Multicenter Randomized Clinical Trial (STEMIRADIAL) in 707 patients.11 Although the direct association between the radial access and mortality may still be doubtful, the significantly lower risk of vascular and bleeding complications should promote the TRA as the preferred access site for most operators.12 Proper training and enough experience are necessary to achieve the optimal results that should receive the strongest level of evidence A in the upcoming guidelines.
Routine Manual Thrombus Aspiration (Class IIa, Level of Evidence B)
Recently, the Thrombus Aspiration during Percutaneous coronary intervention in Acute myocardial infarction study (TAPAS) was the only randomised trial showing  the clinical benefit of routine thrombus aspiration versus conventional primary PCI. The mortality at oneyear, as the secondary and not pre-specified clinical endpoint, was found less frequently in the manual thrombus aspiration group (3.6 versus 6.7 %, p=0.018).13,14 The concerns about the single-centre experience and the technique of conventional PCI (balloon predilation before stenting) seem to be even more relevant after the first largescale international multicentre randomised Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia (TASTE) trial published by Fröbert et al.15 This trial reflects the real-world practice using a unique enrolment of patients from the national comprehensive Swedish Coronary Angiography and Angioplasty Registry (SCAAR registry) and endpoints evaluation through national registries without losing a single patient to follow-up. The clot aspiration in comparison with the balloon treatment in 7,244 STEMI patients did not show any statistical difference in mortality as the primary endpoint at 30 days (3.0 versus 2.8 %; p=0.63). This finding was consistent across all pre-specified subgroups and no difference was observed in therate of secondary endpoints obtained from the Swedish Websystem for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART) registry and the national discharge registry (30-day rates of hospitalisation for recurrent myocardial infarction, stent thrombosis, target vessel revascularisation, target lesion revascularisation, and the composite of all-cause mortality or recurrent myocardialinfarction). Currently, the routine manual thrombus aspiration seems to be not supported by the evidence and should be used only selectively. The data from the ongoing Trial of Routine Aspiration Thrombectomy With Percutaneous Coronary Intervention (PCI) Versus PCI Alone in Patients With ST-Segment Elevation Myocardial Infarction (STEMI) Undergoing Primary PCI (TOTAL) with more than 10,000 patients (ClinicalTrials.gov: NCT01149044) will probably have a definite impact on the indication of routine thrombus aspiration during STEMI.16
the clinical benefit of routine thrombus aspiration versus conventional primary PCI. The mortality at oneyear, as the secondary and not pre-specified clinical endpoint, was found less frequently in the manual thrombus aspiration group (3.6 versus 6.7 %, p=0.018).13,14 The concerns about the single-centre experience and the technique of conventional PCI (balloon predilation before stenting) seem to be even more relevant after the first largescale international multicentre randomised Thrombus Aspiration in ST-Elevation Myocardial Infarction in Scandinavia (TASTE) trial published by Fröbert et al.15 This trial reflects the real-world practice using a unique enrolment of patients from the national comprehensive Swedish Coronary Angiography and Angioplasty Registry (SCAAR registry) and endpoints evaluation through national registries without losing a single patient to follow-up. The clot aspiration in comparison with the balloon treatment in 7,244 STEMI patients did not show any statistical difference in mortality as the primary endpoint at 30 days (3.0 versus 2.8 %; p=0.63). This finding was consistent across all pre-specified subgroups and no difference was observed in therate of secondary endpoints obtained from the Swedish Websystem for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies (SWEDEHEART) registry and the national discharge registry (30-day rates of hospitalisation for recurrent myocardial infarction, stent thrombosis, target vessel revascularisation, target lesion revascularisation, and the composite of all-cause mortality or recurrent myocardialinfarction). Currently, the routine manual thrombus aspiration seems to be not supported by the evidence and should be used only selectively. The data from the ongoing Trial of Routine Aspiration Thrombectomy With Percutaneous Coronary Intervention (PCI) Versus PCI Alone in Patients With ST-Segment Elevation Myocardial Infarction (STEMI) Undergoing Primary PCI (TOTAL) with more than 10,000 patients (ClinicalTrials.gov: NCT01149044) will probably have a definite impact on the indication of routine thrombus aspiration during STEMI.16
Periprocedural Pharmacotherapy
Based on the STEMI Guidelines, the dual antiplatelet therapy (Aspirin and an adenosine diphosphate [ADP] receptor blocker) is recommended together with parenteral anticoagulant as early as possible before angiography1 (i.e. immediately after the diagnosis of STEMI is confirmed). The novel agents, prasugrel or ticagrelor, should be preferred over clopidogrel17,18,19 in combination with bivalirudin,20 enoxaparin21 or unfractionated heparin.22 The use of glycoprotein IIb/IIIa inhibitors is indicated only as bailout in high-risk clinical situations, like the presence of large thrombus burden and no-flow phenomenon after PCI. The potential advantage of intracoronary administration of abciximab has been studied but the results have to be confirmed.23 Combination ofthe administration of potent drugs requires an individualised approach with respect to a patient´s risk profile (prothrombotic versus bleeding), complexity of coronary pathology, selected interventional strategy and a good clinical judgement.24 Recommendation of the ESC and ACC/AHA are shown in Tables 1 and 2.
Revascularisation Strategy for ST-segment Elevation Myocardial Infarction with Multivessel Disease
Culprit-only PCI has been recommended in STEMI patients except for patients in cardiogenic shock and continuous ischaemia despite successful infarct-related artery treatment.1 Recently, Wald et al. enrolled 465 patients with STEMI, multivessel disease and primary PCI of the infarct-related artery in the Randomized Trial of Preventive Angioplasty in Myocardial Infarction (PRAMI).25 The patients were randomly assigned to either preventive or no preventive PCI of the non-culprit vessels with at least 50 % stenoses. The study was stopped preliminary because of a highly significant decrease of the composite of death from cardiac causes, non-fatal myocardial infarction, or refractory angina in the preventive PCI group of patients (hazard ratio [HR] 0.35; p<0.001). Hazard ratios for the three components of the primary outcome were 0.34; 0.32 and 0.35, respectively. We are dealing with an exciting finding that needs further investigation. One of the unanswered questions in STEMI patients is the additional value of the functional revascularisation concept based on the fractional flow reserve measurement (ongoing Comparison Between Fractional Flow Reserve Guided Revascularization Versus Conventional Strategy in Acute STEMI Patients With multivessel disease [COMPARE-ACUTE] trial, ClinicalTrials.gov: NCT01399736).