Challenges with Current Balloon-expandable Stents
Vessel lumen sizes are often variable, whereas balloon-expandable stents are tubular by nature. Thus, conventional stents are not able to adapt effectively to atypical coronary anatomy; such as in ectatic or aneurysmal vessels, or in tapered vessels.5,7,8 Currently, the proximal 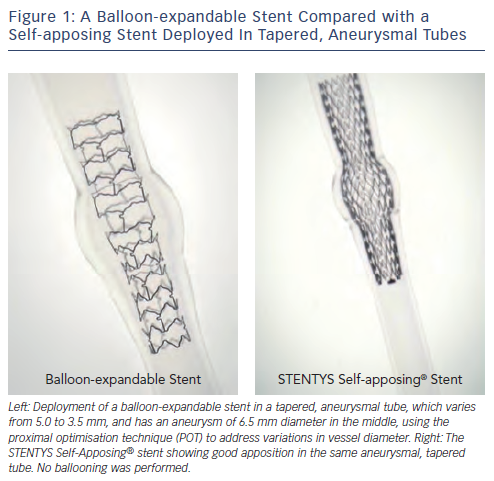 optimisation technique (POT) is used in tapered vessels to try to overcome this restriction. It involves sizing the stent to the distal vessel and then overinflating the proximal segment of the stent with an oversized balloon in a two-step process. This technique is particularly common in the treatment of bifurcation lesions, especially of the left main coronary artery (LMCA).8 The challenge remains when diameter variations are large or varying, due to the subsequent deformation of the stent structure or the inability of the stent to achieve apposition.9
Figure 1 shows the result of a balloon-expandable stent deployed in a tapered, aneurysmal tube, after the POT was applied.
optimisation technique (POT) is used in tapered vessels to try to overcome this restriction. It involves sizing the stent to the distal vessel and then overinflating the proximal segment of the stent with an oversized balloon in a two-step process. This technique is particularly common in the treatment of bifurcation lesions, especially of the left main coronary artery (LMCA).8 The challenge remains when diameter variations are large or varying, due to the subsequent deformation of the stent structure or the inability of the stent to achieve apposition.9
Figure 1 shows the result of a balloon-expandable stent deployed in a tapered, aneurysmal tube, after the POT was applied.
Vessels with a large thrombus burden, such as a SVG or in patients with STEMI, carry the risk of distal embolisation when stenting with a balloon-expandable stent due to balloon-deployment from the centre of the stent towards the outside, high-pressures which squeeze out the thrombus, and large cell sizes through which thrombus may prolapse.6,10 In addition, thrombotic vessels often pose a challenge for the operator to accurately identify the appropriate stent size.10
Similarly, in a CTO situation, there is a transient impairment of vasomotor function post-recanalisation and thus there is limited vessel response to intracoronary nitrates making stent size selection more challenging.11
Using high deployment pressures during stent deployment risks perforation, media injury or necrotic core prolapse. However, positive remodelling post-procedure is common after STEMI and CTO primarily due to vasodilation, but also thrombus dissolution after STEMI.10,12,13 In fact, 70 % of CTOs treated have shown luminal gain in the first eight months.12 Stent oversizing and using higher pressures with balloon-expandable stents is a common technique to minimise subsequent malapposition. Despite the use of this technique, the Randomized Comparison Between the STENTYS Self-Expanding Coronary Stent and a Balloon-expandable Stent in Acute Myocardial Infarction study (APPOSITION II) showed a stent malapposition rate of 28 % for balloon-expandable stents at three days post-primary PCI for STEMI.10
Treatment of bifurcation lesions with balloon-expandable stents continues to have a higher risk of restenosis and stent thrombosis than stenting a simple vessel. Questions still remain regarding these tapered vessels; such as stent sizing, covering the ostium of the side branch, malapposition in the main branch when treating the side branch, as well as stent strut deformation and its effect on the integrity of the stent structure and on drug delivery.4,5,7
The STENTYS Self-Apposing® Stent
The STENTYS BMS and DES(P) stents are self-expanding stents made out of nitinol, a nickel-titanium alloy. They have a memory shape such that the stent self-deploys gently and atraumatically without the need for a deployment balloon. Due to its super-elastic properties and short stent struts, the stent platform is also self-apposing and conforms to the shape of the vessel in which is it is deployed, allowing for a more anatomical fit (see Figure 1).10,13
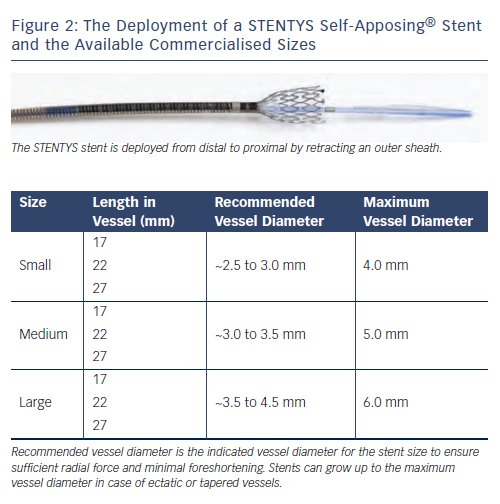
The stent is deployed by retracting a sheath, which releases the stent gradually from distal to proximal in a flower-like shape (see Figure 2). The stent expands until it reaches the vessel wall, and exerts a continuous, gentle outward force onto the wall of the vessel, such that any positive remodelling over time would be accommodated by the stent through subsequent expansion.10,13
The available sizes for the STENTYS BMS and DES(P) can be seen in Figure 2. Each size is flexible enough to cover a range of indicated vessel diameters, and can even grow beyond this size in case of positive remodelling or extreme tapering.
In addition to its self-apposing design, the STENTYS stent contains small, disconnectable bridges all along the stent, which can be disconnected to provide an opening to the side branch. A percutaneous transluminal coronary angioplasty (PTCA) balloon is inflated at low pressures within the distal cell to disconnect several bridges around the side branch to create access. The stent then self-expands into the side branch, thus providing a flap to cover ostial side branch disease.
The instructions for use (IFU) for the STENTYS BMS and DES(P) lists the stent indications as: improving coronary luminal diameter in native coronary arteries and coronary bypass grafts in the treatment of acute coronary syndrome (ACS); de novo lesions in vessels involving a side branch (bifurcation); and de novo lesions in vessels with diameter variations (e.g. tapered, ectatic).