STENTYS Cases in Atypical Coronary Anatomy
Left Main Bifurcation
A male patient of 73 years with three hours of chest pain presented at the catheterisation laboratory with STEMI.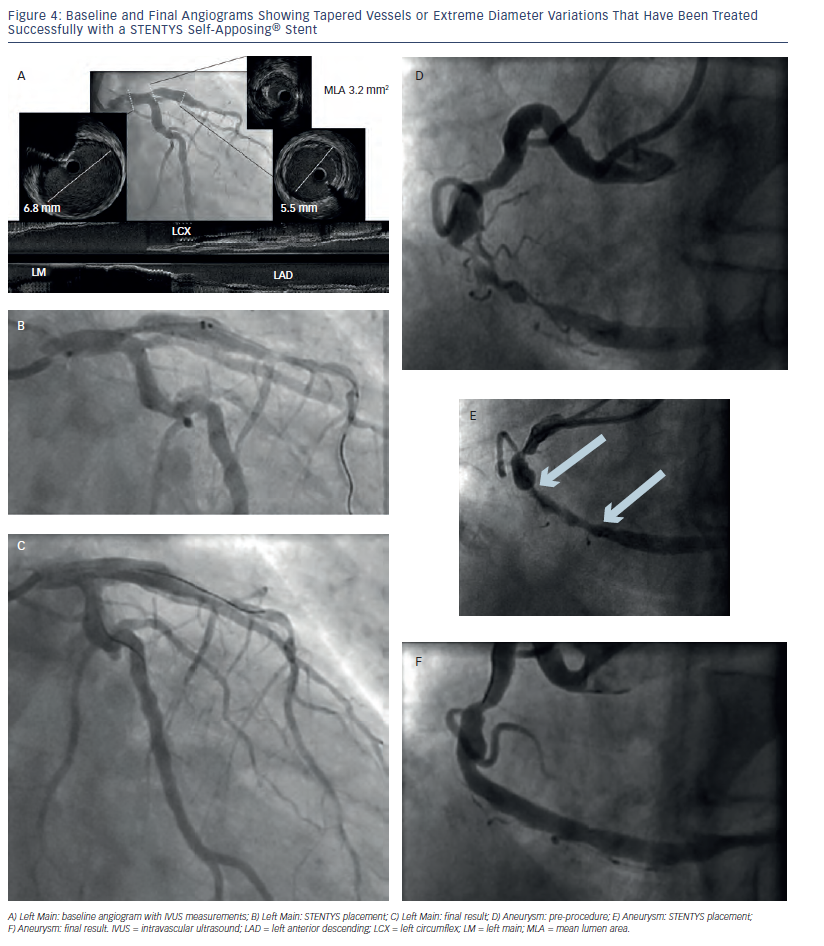 Diagnostic angiography showed Thrombolysis In Myocardial Infarction (TIMI) I flow in the anterolateral (AL) region with a suspected ostial lesion in the left anterior descending (LAD) artery. Upon examination with intravascular ultrasound (IVUS), it was found that the left main (LM) measured 6.8 mm and the proximal LAD measured 5.6 mm. At the level of the stenosis, there was a mean lumen area (MLA) of 3.2 square millimetres (see Figure 4a). The AL branch was treated with two XIENCE PRIME stents (Abbott Vascular, Santa Clara, CA, US) of sizes 2.25 x 18.00 mm and 2.25 x 12.00 mm in an overlapping manner. The LM/LAD arteries were pre-dilated with a TREK 3.0/12.0 mm semi-compliant balloon (Abbott Vascular). Due to the varying vessel diameters along the lesion, the very large diameters of the LM and LAD, and to prevent undersizing and malapposition especially in the LM, a self-apposing STENTYS stent (STENTYS SA, Paris, France) was selected to stent the lesion. A STENTYS DES(P) 3.5-4.5/27.0 mm can grow to over 6.0 mm in tapered vessels, and can also be disconnected at a side branch in bifurcation cases thus avoiding strut deformation. The stent was positioned (see Figure 4b) and deployed, and subsequent post-dilation was performed with a 5.0 mm balloon within the stent. A balloon was tracked through the most distal cell into the left circumflex (Cx) artery where it was inflated between the struts, resulting in a disconnection of the stent bridges and an opening of the stent towards the circumflex. The final result was astonishing (see Figure 4c) and the post-procedure result was maintained out to three months.
Diagnostic angiography showed Thrombolysis In Myocardial Infarction (TIMI) I flow in the anterolateral (AL) region with a suspected ostial lesion in the left anterior descending (LAD) artery. Upon examination with intravascular ultrasound (IVUS), it was found that the left main (LM) measured 6.8 mm and the proximal LAD measured 5.6 mm. At the level of the stenosis, there was a mean lumen area (MLA) of 3.2 square millimetres (see Figure 4a). The AL branch was treated with two XIENCE PRIME stents (Abbott Vascular, Santa Clara, CA, US) of sizes 2.25 x 18.00 mm and 2.25 x 12.00 mm in an overlapping manner. The LM/LAD arteries were pre-dilated with a TREK 3.0/12.0 mm semi-compliant balloon (Abbott Vascular). Due to the varying vessel diameters along the lesion, the very large diameters of the LM and LAD, and to prevent undersizing and malapposition especially in the LM, a self-apposing STENTYS stent (STENTYS SA, Paris, France) was selected to stent the lesion. A STENTYS DES(P) 3.5-4.5/27.0 mm can grow to over 6.0 mm in tapered vessels, and can also be disconnected at a side branch in bifurcation cases thus avoiding strut deformation. The stent was positioned (see Figure 4b) and deployed, and subsequent post-dilation was performed with a 5.0 mm balloon within the stent. A balloon was tracked through the most distal cell into the left circumflex (Cx) artery where it was inflated between the struts, resulting in a disconnection of the stent bridges and an opening of the stent towards the circumflex. The final result was astonishing (see Figure 4c) and the post-procedure result was maintained out to three months.
Aneurysmal vessel
A 76-year-old male with a history of PCI of the LAD in 1990 (anteroseptal infarction), and a 2012 echocardiogram showing akinesia of the apex, and anterior and lateral walls, presented with a non-STEMI (NSTEMI). He was known to have had transient ischaemic attacks (TIAs) and hypertension. The baseline angiogram showed a large aneurysmal right coronary artery (RCA) with long, significant stenoses (see Figure 4d). It is technically challenging to appose balloon-expandable stents to ectatic, aneurysmal, large vessels such as this one, and thus treatment with a STENTYS stent was chosen. Pre-dilation was performed using a TREK balloon (Abbott Vascular) of size 3.0/10.0 mm at 10 atmospheres (atm). A STENTYS 3.5-4.5/27.0 mm was subsequently positioned (see Figure 4e) and deployed over the lesion, followed by post-dilation with a 4.5/20.0 mm balloon at 10 atm. The final angiogram showed an optimal result (see Figure 4f). At six months, the patient had no events and was angina-free.
Saphenous Vein Graft
A 53-year-old male patient had a history of an inferior-posterior infarct in 1993 and coronary artery bypass grafting (CABG) in 1994. In 2010, his left internal 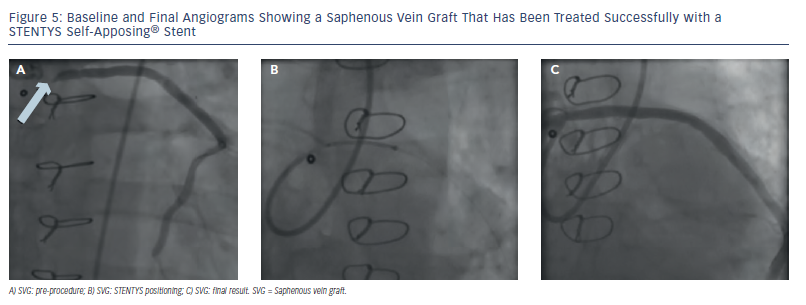 mammary artery (LIMA) to the LAD was found to be patent, but a SVG was occluded at the distal anastomosis. In 2011, he was a participant in stem cell therapy. The patient presented with severe anginal complaints with Canadian Cardiovascular Society (CCS) grade 3/4, despite extensive anti-anginal medication. A coronary angiogram revealed a 100 % occluded RCA and left coronary artery (LCA), a patent LIMA to the LAD with collaterals to the RCA, and a significant ostial lesion in the distally occluded SVG (see Figure 5a). The challenge of this case was the ostial location of the lesion and the risk of distal embolisation. The lumen diameter was quite large, increasing the risk of possible undersizing. A self-apposing stent was considered due to its deployment from distal to proximal, which could limit the risk of distal embolisation, and its ability to provide better apposition of this large, irregular venous contour, even after resolution of thrombus/ debris following PCI. A 6-French guiding catheter with good support was selected (Multipurpose (MP) 2.0). After pre-dilation, a STENTYS DES(P) 3.5-4.5/22.0 mm was positioned at the ostium of the SVG (see Figure 5b) and deployed. Post-dilation of the ostium was performed with a 3.0/12.0 mm Maverick balloon (Boston Scientific, Natick, MA, US) at 16 atm. The entire stent was then post-dilated with a 4.5/8.0 mm Quantum Apex non-compliant balloon (Boston Scientific) at 12-16 atm. The final angiogram showed a good result (see Figure 5c).
mammary artery (LIMA) to the LAD was found to be patent, but a SVG was occluded at the distal anastomosis. In 2011, he was a participant in stem cell therapy. The patient presented with severe anginal complaints with Canadian Cardiovascular Society (CCS) grade 3/4, despite extensive anti-anginal medication. A coronary angiogram revealed a 100 % occluded RCA and left coronary artery (LCA), a patent LIMA to the LAD with collaterals to the RCA, and a significant ostial lesion in the distally occluded SVG (see Figure 5a). The challenge of this case was the ostial location of the lesion and the risk of distal embolisation. The lumen diameter was quite large, increasing the risk of possible undersizing. A self-apposing stent was considered due to its deployment from distal to proximal, which could limit the risk of distal embolisation, and its ability to provide better apposition of this large, irregular venous contour, even after resolution of thrombus/ debris following PCI. A 6-French guiding catheter with good support was selected (Multipurpose (MP) 2.0). After pre-dilation, a STENTYS DES(P) 3.5-4.5/22.0 mm was positioned at the ostium of the SVG (see Figure 5b) and deployed. Post-dilation of the ostium was performed with a 3.0/12.0 mm Maverick balloon (Boston Scientific, Natick, MA, US) at 16 atm. The entire stent was then post-dilated with a 4.5/8.0 mm Quantum Apex non-compliant balloon (Boston Scientific) at 12-16 atm. The final angiogram showed a good result (see Figure 5c).
Chronic Total Occlusion
A male patient of 74 years had a history of PCI of a diagonal in 2002, a coronary angiogram revealing a CTO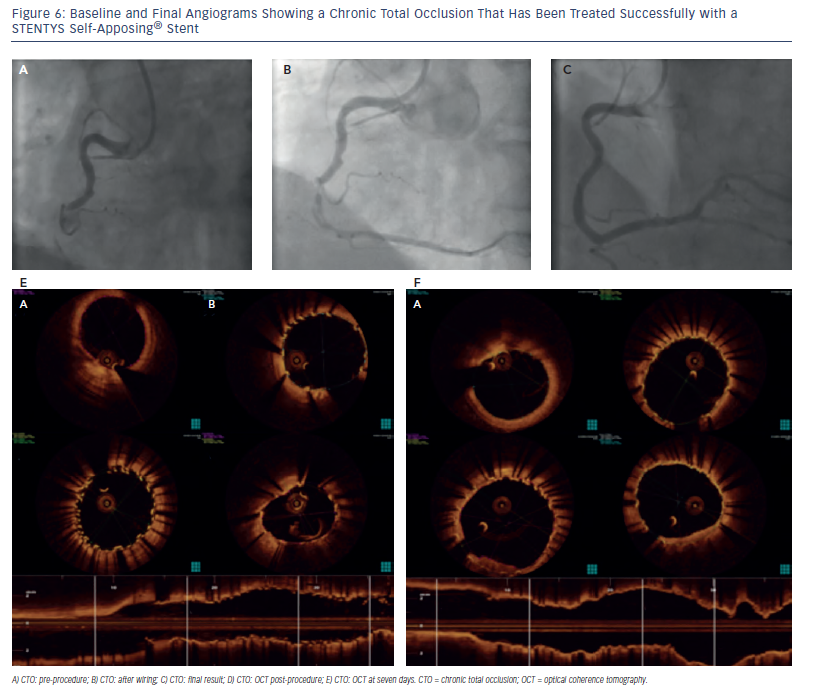 of the RCA and a 90 % stenosis of the Cx in 2011, and PCI of the Cx in 2012. He presented with severe anginal complaints, with CCS grade 3/4 despite extensive anti-anginal medication. Angiography was performed via the radial artery and a CTO of the mid-RCA was confirmed (see Figure 6a). No significant stenoses were found in the LCA, and there were small collaterals to the posterior descending artery (PDA). An Amplatz Left 2.0 (AL2) guiding catheter (Cordis Corporation, a Johnson & Johnson company, Miami Lakes, FL, US) was chosen for good backup with a Pilot 50/150 wire (Abbott Vascular), and the occlusion was crossed (see Figure 6b). Pre-dilation was performed with incremental balloon diameters starting at 1.25 mm, then 2.00 mm and then 2.50 mm to restore flow. Due to concern about the actual vessel size post-recanalisation and the risk of long-term malapposition, stent thrombosis and repeat PCI or restenosis, the STENTYS technology was selected. STENTYS DES(P) stents of sizes 3.0-3.5/27.0 mm and 3.0-3.5/22.0 mm were placed proximally and distally, respectively, in an overlapping manner. Both stents were post-dilated with a Quantum Apex (Boston Scientific) non-compliant balloon of size 3.5/15.0 mm at 14 atm. Optical coherence tomography (OCT) confirmed good stent apposition to the vessel wall (see Figure 6d), and the final angiogram showed an optimal result (see Figure 6c). At seven days post-procedure, the patient underwent another coronary angiogram, which showed a sustained optimal result. OCT at seven days (see Figure 6e) revealed an increase in minimum lumen area of 11 % since post-procedure. One year later, the patient was performing heavy physical exercise on his horse farm without anginal complaints.
of the RCA and a 90 % stenosis of the Cx in 2011, and PCI of the Cx in 2012. He presented with severe anginal complaints, with CCS grade 3/4 despite extensive anti-anginal medication. Angiography was performed via the radial artery and a CTO of the mid-RCA was confirmed (see Figure 6a). No significant stenoses were found in the LCA, and there were small collaterals to the posterior descending artery (PDA). An Amplatz Left 2.0 (AL2) guiding catheter (Cordis Corporation, a Johnson & Johnson company, Miami Lakes, FL, US) was chosen for good backup with a Pilot 50/150 wire (Abbott Vascular), and the occlusion was crossed (see Figure 6b). Pre-dilation was performed with incremental balloon diameters starting at 1.25 mm, then 2.00 mm and then 2.50 mm to restore flow. Due to concern about the actual vessel size post-recanalisation and the risk of long-term malapposition, stent thrombosis and repeat PCI or restenosis, the STENTYS technology was selected. STENTYS DES(P) stents of sizes 3.0-3.5/27.0 mm and 3.0-3.5/22.0 mm were placed proximally and distally, respectively, in an overlapping manner. Both stents were post-dilated with a Quantum Apex (Boston Scientific) non-compliant balloon of size 3.5/15.0 mm at 14 atm. Optical coherence tomography (OCT) confirmed good stent apposition to the vessel wall (see Figure 6d), and the final angiogram showed an optimal result (see Figure 6c). At seven days post-procedure, the patient underwent another coronary angiogram, which showed a sustained optimal result. OCT at seven days (see Figure 6e) revealed an increase in minimum lumen area of 11 % since post-procedure. One year later, the patient was performing heavy physical exercise on his horse farm without anginal complaints.