Stroke
Neurological sequelae following TAVI remain highly debated, and the adverse event most feared by patients and their families. Thromboembolic events with cerebrovascular injury may occur at various stages during the TAVI procedure itself (retrograde crossing of the calcified aortic valve, preliminary valvuloplasty, manipulation of the delivery catheter through the aortic arch and valve deployment)15 and may also arise as a result of other post-procedural influences (e.g. atrial fibrillation [AF]). As yet, there is no accepted or evidence-based guidance as to the optimal peri- and post-procedural anti-platelet or anticoagulant regime. However, the ongoing Aspirin versus aspirin and clopidogRel following Transcatheter aortic valvE implantation (ARTE) pilot trial will provide some useful data.
The PARTNER A trial of TAVI versus surgical AVR in high-risk patients with symptomatic aortic stenosis16 showed that the incidence of all stroke and transient ischaemic attack (TIA) following TAVI was 5.5 % at 30 days and 8.3 % at 1 year, and 3.8 % and 5.1 %, respectively, for major stroke. In the surgical arm, all stroke and TIA incidence was 2.4 % and 4.3 % at 30 days and 1 year, respectively, and 2.1 % and 2.4 % for major stroke. These data, suggesting an early excess of stroke following TAVI, were balanced by longer-term follow-up data showing equivalent stroke rates at 36 months (8.2 % versus 9.3 %, respectively, p=0.763).
In the PARTNER B trial,6 patients deemed unsuitable for surgery due to comorbidities associated with a predicted probability of 50 % of death after surgery, were randomised to undergo TAVI or continue with medical therapy. There was a significant reduction in mortality associated with TAVI at 1-year follow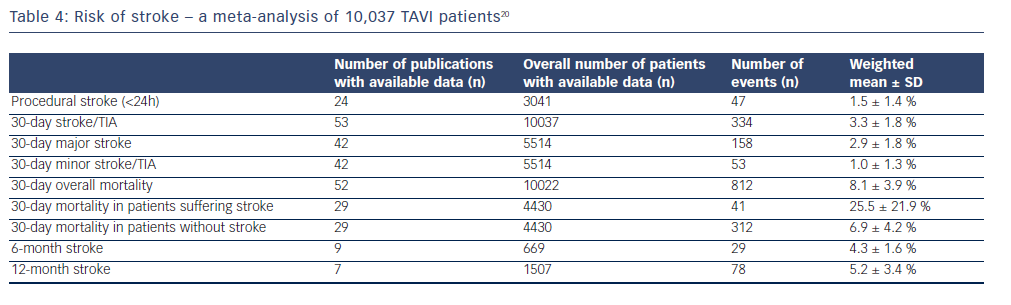 up (30.7 % versus 50.7 %, hazard ratio [HR] 0.58; 95 % confidence interval [CI] 0.43 to 0.78; p<0.001) although major strokes were more common in the TAVI group (5.0 % versus 1.1 % at 30 days; p=0.06; 7.8 % versus 3.9 % at 1 year; p=0.18).
up (30.7 % versus 50.7 %, hazard ratio [HR] 0.58; 95 % confidence interval [CI] 0.43 to 0.78; p<0.001) although major strokes were more common in the TAVI group (5.0 % versus 1.1 % at 30 days; p=0.06; 7.8 % versus 3.9 % at 1 year; p=0.18).
A small study conducting diffusion-weighted magnetic resonance imaging (MRI) scans to detect subclinical cerebral ischaemic post-TAVI with CoreValve valves identified that silent cerebral embolism is frequent (73 %) compared with the incidence of clinically apparent cerebral embolism (3.6 %).17 This high subclinical uncovering was again shown in a small study that carried out neurological testing and serial cerebral diffusion weighted MRI at baseline, at 3.4 days (2.5-4.4) post-procedure and at 3 months. New ischaemic lesions were identified in 84 % of cases, which is considerably more when compared with 48 % of sAVR patients, and were usually multiple but smaller than after sAVR. No patients were symptomatic, there was no demonstrable neurocognitive impairment and no further events were reported at 3 months.18
A meta-analysis of TAVI versus sAVR derived from 14 studies found no significant difference in stroke risk, either at the time of the procedure (2.6 % versus 2.3 %, relative risk [RR] 1.16, 95 % CI 0.72-1.87; p=0.54) or at 1-year follow up (4.5 % versus 3.4 %, RR 1.27, 95 % CI 0.68-2.37; p=0.46).19 However, a subgroup analysis of two randomised controlled trials did identify higher incidence of stroke/TIAs associated with TAVI (5.8 % versus 2.3 %; p=0.02).
In a prospective single-centre registry (Bern TAVI registry) of 389 high-risk elderly patients with severe symptomatic aortic stenosis undergoing TAVI from August 2007 to October 2011, 14 patients (3.6 %) experienced at least one stroke (major in 3.1 %; minor in 0.5 %) and 71.4 % of these occurred within 1 day of the procedure.15 Smaller body mass index (BMI 25 adjusted odds ratio [AOR] 0.78 compared with BMI <25), previous stroke (AOR 1.87) and chronic obstructive pulmonary disease (COPD) (AOR 4.73) were all risk factors for cerebrovascular complications. However, conventional risk factors for stroke including age, hypertension, male gender, diabetes mellitus, smoking and AF were not found to have an effect, nor antithrombotic treatment at baseline. Surprisingly, the number of aortic valve pre-dilatations was not associated with a higher incidence of stroke, whereas the converse is true with post-dilatation (AOR 2.00). Significant risk was also associated with more than one implantation attempt (AOR 8.32). All-cause mortality at 30 days was significantly higher in the group who suffered a stroke (42.3 % versus 5.1 %, OR 11.7, 95 % CI 3.4-40.3; p<0.001) with cardiovascular mortality accounting for 38.4 % in the stroke group, and 4.6 % in the group with no neurological consequences.
Similarly, a higher 30-day mortality was associated with stroke in a meta-analysis including 10,037 patients undergoing TAVI between January 2004 and November 2011.20 Here, procedural stroke (<24 hours) occurred in 1.5+/-1.4 %, increasing to 3.3+/-1.8 % at 30 days, 4.3+/-1.6 % at 6 months and 5.2+/- 3.4 % at 1 year. Table 4 shows the incidence of stroke and associated mortality.
In a 5-year follow-up period, cumulative major ischaemic stroke rates were 9.7 % and haemorrhagic stroke rates 7.3 % (50 % fatal). The calculated annual risk of ischaemic stroke was consistently around 2 %, whereas the risk of haemorrhagic stroke increased each year, being 2.8 % in the first year, and reaching 7.3 % in years 4 and 5.14