Mitral Leaflets
The anterior leaflet tends to be the more mobile of the two leaflets, while the posterior leaflet acts as the support structure.17 The anterior mitral leaflet is in fibrous continuity with the aortic valve, bordered on either side by the right and left fibrous trigones. The areas of both leaflets are identical, with the posterior leaflet being broad (occupying nearly two-thirds of the annular circumference) and short.1 Leaflet defects typically include excessive/deficient tissue or unrestrained/ restricted mobility. The goal of treating the mitral leaflets is to improve leaflet coaptation and to reduce the effective regurgitant orifice area.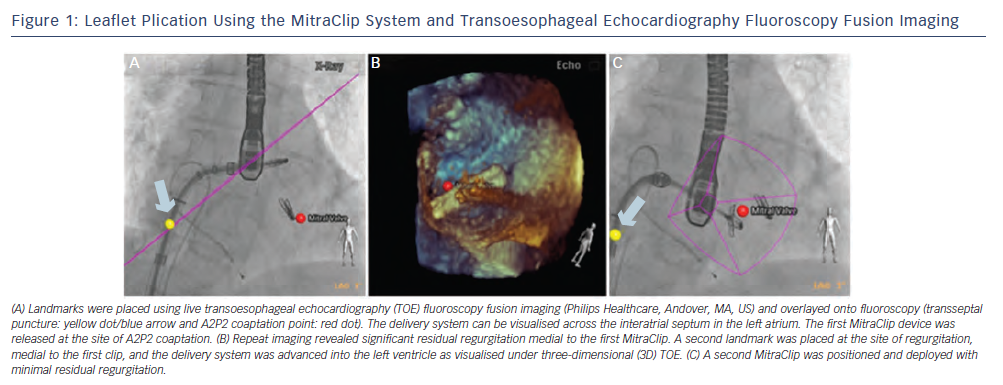
Leaflet Plication
Based on the surgical Alfieri technique, percutaneous leaflet plication re-establishes leaflet coaptation by approximating the anterior and posterior leaflets (A2 and P2 central segments, site of regurgitation) together via a cobalt-chromium clip.18 The MitraClip system (Abbott Vascular, Redwood City, CA, US) creates an effective double-orifice mitral valve, reducing the overall amount of MR for both functional and degenerative types. The system uses a steerable catheter (24F proximally, 22F distally) to deliver the MitraClip transseptally and allow for grasping of the leaflet free edges.19 The MR jet must be centrally located with sufficient coaptation length of at least 2 mm, a depth from the MA of no more than 11 mm, and if a flail leaflet is present, a gap and flail width not exceeding 10 mm and 15 mm, respectively.
MitraClip implantation is typically guided by conventional fluoroscopy and transoesophageal echocardiography (TOE). The use of live three-dimensional (3D) TOE-fluoroscopy fusion technology (EchoNavigator system [Philips Healthcare, Andover, MA, US]) can potentially further aid in implantation. With this technology, landmarks can be placed at the site of transseptal puncture (3-4 centimetres [cm] above the coaptation plane) and at the central A2P2 coaptation or intended coaptation point (if prolapse or a flail leaflet is present) to guide the intervention (see Figure 1a). The device can be steered until it is aligned over the landmark and advanced into the LV (see Figure 1b). The clip is then retracted for leaflet grasping and device closure. The MitraClip can be repositioned or removed prior to final deployment and multiple clips can be implanted to achieve the desired MR reduction (see Figure 1c).
The Endovascular Valve Edge-to-Edge Repair Study (EVEREST) II study enrolled 279 patients with moderate-severe or severe MR in a 2:1 ratio to undergo either MitraClip implantation or conventional mitral valve repair or replacement.20 Successful reduction in MR by at least 1 grade was achieved in 76 % of patients. Composite endpoint of freedom from death, MV surgery or reoperation, and MR >2+ at one year was 72.4 % and 87.8 % (p=0.02), MitraClip and surgery, respectively, in patients with successful in-hospital results. The MitraClip was associated with a significant improvement in New York Heart Association (NYHA) classification with superiority in safety endpoints, major adverse events occurring in 15 versus 48 % at 30 days (p<0.001), compared with surgery. Similar results were achieved regardless of the MR type and were maintained at three years. In those requiring surgery, it usually occurred within six months after implantation and surgical options were preserved with 84 % able to undergo successful mitral valve repair.21
Leaflet Coaptation
Providing a sealing surface for the leaflets, the Mitra-Spacer™ (Cardiosolutions Inc., Stoughton, MA, US) is a polyurethane-silicone polymer spacer that positions itself at the zone of coaptation, filling the regurgitant orifice. It is anchored to the apex and can be delivered via a transseptal or transapical approach. Pre-sizing balloons are used to appropriately match the spacer to the dimension of the mitral valve (MV) orifice. The device does not alter the MV apparatus and can be fully removed or maintained permanently. Potential complications with the system include thrombus formation or iatrogenic mitral stenosis. The FIM trial resulted in a 1-2 grade reduction in MR without a significant transmitral gradient.22