How to Ensure Procedural Safety and Good Long-term Results in Complex Coronary CTO Procedures
Professor Ahmed Khashaba of Cairo, Egypt presented the factors that should be considered before performing a CTO procedure. First, it is essential to select the right patient, keeping in mind that the expected benefit of a CTO procedure must exceed the negative consequences. It is also important to take the age of the patient into account, as well to assess the level of anti-ischaemic medical therapy received, the symptom status and the ischaemic burden. According to current guidelines, percutaneous recanalization of CTOs should be considered in patients with expected ischaemia reduction in a corresponding myocardial territory and/or angina relief.1 In addition, retrograde recanalisation of CTOs may be considered after a failed antegrade approach or as the primary approach in selected patients. In a meta-analysis comparing successful and failed PCI for CTO, successful PCI recanalisation of a CTO was associated with improved long-term clinical outcomes.2 In another meta-analysis, successful recanalisation was associated with a significant reduction in the rate of residual/recurrent angina.3
Good preparation is essential for performing CTO procedures. Preprocedural imaging should include myocardial perfusion imaging to assess ischaemia and myocardial viability, and multiple detector computed tomography to determine the 3D vessel course in the occluded segment, the length and composition of the CTO, and the distal vessel size and remodelling. Pre-procedural medications should comprise standard dual antiplatelet (DAPT) and anti-ischaemic therapy. Strategies to prevent contrast-induced nephropathy should also be considered; these include discontinuing any nephrotoxic drugs, intravascular volume expansion and administering a predefined maximum radiographic contrast dose (4 ml x body weight [kg]/serum creatinine [mg/dl]).
Radiation dose management is essential as radiation injury can lead to severe consequences for the patient, ranging from erythema that resolves in hours to ulceration that can take >6 weeks to heal; therefore, the patient should not undergo a repeat procedure prematurely.
It is also important to tai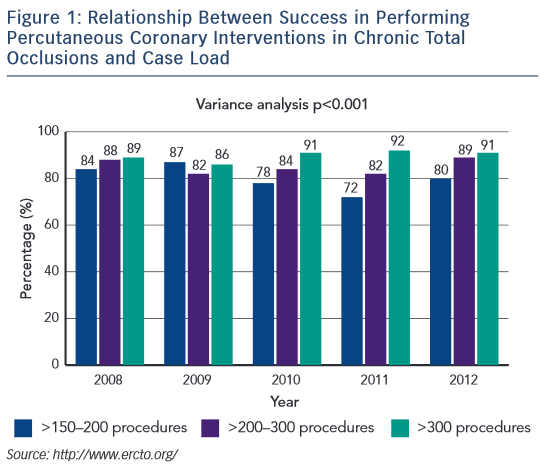 lor the case selection to the level of experience of the operator. A Level C operator (i.e. having undertaken <500 PCIs) should only perform PCI of simple lesions and simple bifurcations. A Level B operator (500–1000 PCIs) may perform more complex procedures including PCI of complex bifurcations, moderate calcified lesions and some cases of CTO. Only a Level A operator (>1000 PCIs, including ≥300 CTOs) should be permitted to perform PCI of difficult cases such as long and highly calcified lesions and complex CTOs, including retrograde approaches. If a Level C operator attempts a Level A task, he/she is less likely to be successful and may cause harm to the patient.4 Data from the European CTO registry shows the correlation between success rate and case load in performing PCI for CTOs (see Figure 1; http://www.ercto.org/).
lor the case selection to the level of experience of the operator. A Level C operator (i.e. having undertaken <500 PCIs) should only perform PCI of simple lesions and simple bifurcations. A Level B operator (500–1000 PCIs) may perform more complex procedures including PCI of complex bifurcations, moderate calcified lesions and some cases of CTO. Only a Level A operator (>1000 PCIs, including ≥300 CTOs) should be permitted to perform PCI of difficult cases such as long and highly calcified lesions and complex CTOs, including retrograde approaches. If a Level C operator attempts a Level A task, he/she is less likely to be successful and may cause harm to the patient.4 Data from the European CTO registry shows the correlation between success rate and case load in performing PCI for CTOs (see Figure 1; http://www.ercto.org/).
Another essential factor in assuring success with CTO procedures is the use of the appropriate approach. A bilateral femoral approach gives a larger lumen for more equipment and better support, but has a higher rate of vascular complications. A bilateral radial approach results in a smaller lumen, less support, higher radiation exposure, but has a lower rate of vascular complications and better patient comfort. A combined femoral and radial procedure is the optimal approach, using a larger sheath/guide than when using an antegrade approach.
It is essential to exert minimal disruption during the PCI procedure. A study assessing the incidence of reocclusion and identification of predictors of angiographic failure after successful CTO, found that a successful subintimal tracking and re-entry technique was associated with a 57 % reocclusion rate.5 However, the use of everolimus-eluting stents was associated with a significantly lower reocclusion rate.
The immediate outcome should be optimised – a final thrombolysis in myocardial infarction flow < grade 3 (TIMI <III) is associated with lower major adverse cardiac event-free survival rate.6 A recent study found that the use of intravascular ultrasound (IVUS)-guided intervention leads to increased post-dilation, balloon pressures and post-procedural minimum lumen diameter, and improved clinical outcomes compared with conventional angiography-guided approaches.7
Finally, stent choice for CTO interventions is crucial; second-generation DES are associated with lower rates of restenosis and re-occlusion compared with first-generation DES.5,8–10 An ideal stent for a complex CTO intervention would be a biodegradable polymer or polymer-free DES with thin struts and vessel conformability, thus resulting in good vessel coverage, low or no longitudinal stent deformation and low restenosis rates.
In conclusion, appropriate pre-procedural planning is key to ensuring high success rates and avoiding unnecessary risk. Optimising the immediate outcome is essential to maintaining long-term patency. This may be facilitated by minimal vessel disruption, and the use of IVUS and second-generation DES. Currently available DES with absorbable polymer may further improve device safety and efficacy.
The publication of this article was supported by Alvimedica.