PCI in a Patient with a Complex Coronary CTO: Procedure and Clinical Outcome
Dr Roberto Garbo of Turin, Italy began his presentation by stating that the availability of DES has greatly improved outcomes in CTO, as the use of BMS has been associated with reva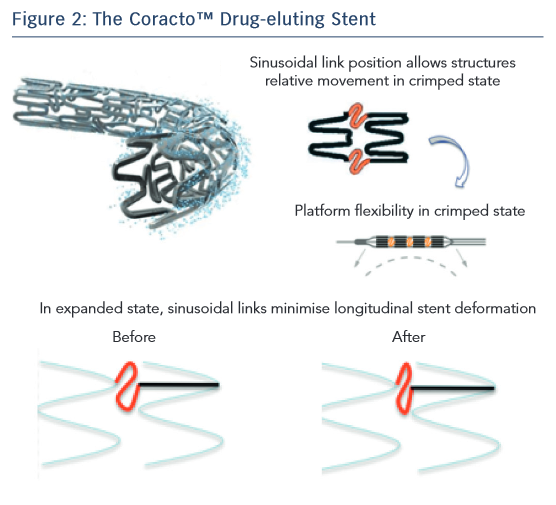 scularisation and restenosis. However, a DES has specific requirements when treating CTO; these include deliverability, stent matching to the vessel and good clinical results at follow-up. In terms of delivery, the Coracto DES features optimised geometry in the ‘crimped’ state owing to its sinusoidal link position that allows flexibility (see Figure 2), thin stent struts (a total strut thickness of 88 μm, lower than other currently available DES) and an optimised delivery system. Next, Dr Garbo considered stent matching to the vessel. The Coracto DES also features optimised geometry in its expanded state, a result of its sinusoidal link shape. Another important consideration is elastic recoil, i.e. the natural reduction in diameter of the stent after deflation of the balloon due to the elasticity of the stent material. Most DES are formed of cobalt-chromium, which has an average recoil of 5–6 %. The Coracto DES is made of stainless steel, which has an average recoil of only 2–3 %.11 Stent recoil has been identified as a significant predictor of late lumen loss (LLL).12 Longitudinal stent deformation is also a crucial factor in matching a stent to a vessel. The sinusoidal shape of the links in the Coracto stent minimises longitudinal deformation. The stent has a maximum expanded cell diameter of 4.0 mm, making it ideal for side-branch crossing.11 Finally, the Coracto DES is designed to optimise clinical outcomes. Preclinical studies indicated that the polymer of the Coracto DES provides controlled release of rapamycin (sirolimus), and degradation of the polymer is completed within 8–10 weeks, leaving a BMS (see Figure 3).13
scularisation and restenosis. However, a DES has specific requirements when treating CTO; these include deliverability, stent matching to the vessel and good clinical results at follow-up. In terms of delivery, the Coracto DES features optimised geometry in the ‘crimped’ state owing to its sinusoidal link position that allows flexibility (see Figure 2), thin stent struts (a total strut thickness of 88 μm, lower than other currently available DES) and an optimised delivery system. Next, Dr Garbo considered stent matching to the vessel. The Coracto DES also features optimised geometry in its expanded state, a result of its sinusoidal link shape. Another important consideration is elastic recoil, i.e. the natural reduction in diameter of the stent after deflation of the balloon due to the elasticity of the stent material. Most DES are formed of cobalt-chromium, which has an average recoil of 5–6 %. The Coracto DES is made of stainless steel, which has an average recoil of only 2–3 %.11 Stent recoil has been identified as a significant predictor of late lumen loss (LLL).12 Longitudinal stent deformation is also a crucial factor in matching a stent to a vessel. The sinusoidal shape of the links in the Coracto stent minimises longitudinal deformation. The stent has a maximum expanded cell diameter of 4.0 mm, making it ideal for side-branch crossing.11 Finally, the Coracto DES is designed to optimise clinical outcomes. Preclinical studies indicated that the polymer of the Coracto DES provides controlled release of rapamycin (sirolimus), and degradation of the polymer is completed within 8–10 weeks, leaving a BMS (see Figure 3).13
Dr Garbo presented a case of a 75-year-old man with effort angina and moderate antero-lateral ischaemia identified by single-ph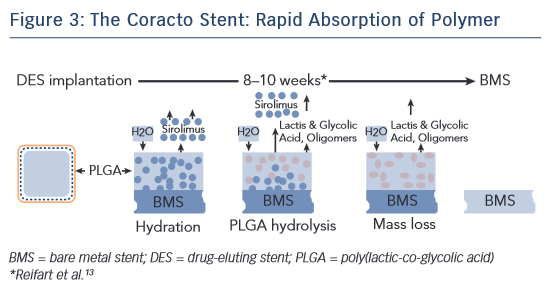 oton emission computerised tomography. A basal angiogram showed LAD ostial occlusion with some collateral flow from the right. The blunt CTO segment and occlusion length of >20 mm resulted in a J-CTO score of 2, which indicates a difficult procedure with reduced success rate (<90 %).14 Treatment of the CTO was by PCI of the ostial LAD with a bilateral femoral approach using a Fielder XT-A guidewire and a Corsair 135 catheter. A contralateral injection was performed to confirm entry into the true lumen, followed by predilation with the microcatheter. IVUS was also used to evaluate the left main (LM) artery. Two stents were implanted: a Coracto 3.0 × 24 mm and a 3.5 × 17 mm on the LM artery. Proximal optimisation technique was performed in the LM artery with an NC 4.0 balloon and a triple kissing balloon 3.5–2.5–2.5 was also needed. Final IVUS confirmed the success of the procedure. At 9 months’ follow-up, angiography and optical coherence tomography (OCT) were performed. Good endothelialisation of all stents was seen with mild in-stent restenosis on the worst area of occlusion (LLL: 0.39 mm).
oton emission computerised tomography. A basal angiogram showed LAD ostial occlusion with some collateral flow from the right. The blunt CTO segment and occlusion length of >20 mm resulted in a J-CTO score of 2, which indicates a difficult procedure with reduced success rate (<90 %).14 Treatment of the CTO was by PCI of the ostial LAD with a bilateral femoral approach using a Fielder XT-A guidewire and a Corsair 135 catheter. A contralateral injection was performed to confirm entry into the true lumen, followed by predilation with the microcatheter. IVUS was also used to evaluate the left main (LM) artery. Two stents were implanted: a Coracto 3.0 × 24 mm and a 3.5 × 17 mm on the LM artery. Proximal optimisation technique was performed in the LM artery with an NC 4.0 balloon and a triple kissing balloon 3.5–2.5–2.5 was also needed. Final IVUS confirmed the success of the procedure. At 9 months’ follow-up, angiography and optical coherence tomography (OCT) were performed. Good endothelialisation of all stents was seen with mild in-stent restenosis on the worst area of occlusion (LLL: 0.39 mm).
In conclusion, complex CTO recanalisation is easier to achieve when using the most appropriate method (e.g. controlateral injection for the visualisation of distal vessels) and adequate materials (microcatheters and dedicated wires). The Coracto DES has unique properties that make it a useful option in treating such challenging lesions, including rapid reabsorption of polymer. It has demonstrated a good safety profile, showing complete endothelialisation of all struts at follow-up OCT evaluation.
The publication of this article was supported by Alvimedica.