Oral Anticoagulation for Stroke Prevention in Patients with Atrial Fibrillation
Vitamin K Antagonists
AF is the most common indication for long-term OAC. AF affects up to 2 % of the general population and as many as 15 % of octogenarians.14–16 Blood stasis within the non-contractile left atrium predisposes these subjects to thromboembolic cerebral infarction, with an average annual stroke rate of about 5 % in non-valvular AF.17 OAC with a vitamin K antagonist (VKA) such as warfarin is highly effective at reducing the risk of stroke in patients with AF. In a meta-analysis of 29 studies, which included 28,044 patients, for example, VKA therapy was associated with a 67 % relative reduction in the rate of ischaemic stroke.18 Warfarin is substantially more effective than aspirin, which reduced the risk of stroke in patients with AF by 22 % in placebo-controlled trials.18,19 Warfarin is also considerably more effective than DAPT at preventing stroke in patients with AF. Atrial Fibrillation Clopidogrel Trial with Irbesartan for prevention of Vascular Events (ACTIVE- W) was stopped early when a clear significant result was demonstrated between patients who were randomly allocated to VKA therapy compared with aspirin and clopidogrel, with an annual rate of stroke, systemic embolus, myocardial infarction (MI) or vascular death of 3.9 % in the VKA group compared with 5.6 % in the DAPT group.5 ACTIVE-A subsequently showed that aspirin and clopidogrel was superior to aspirin alone for stroke prevention in patients with AF with a relative risk reduction of 28 %.20 Discontinuation of OAC in patients with AF, even temporarily, is associated with an increased stroke risk.5
Non-vitamin K Antagonist Oral Anticoagulants
NOACs such as the direct thrombin inhibitor, dabigatran and the factor Xa inhibitors, rivaroxaban and apixaban, have recently em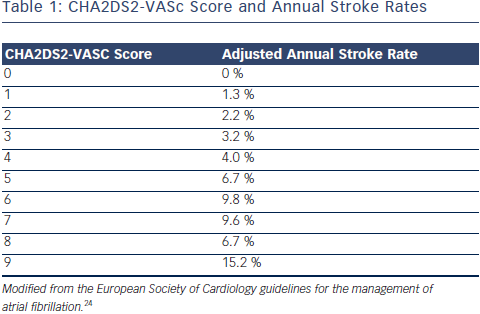 erged as alternatives to warfarin for stroke prevention in patients with AF. When compared with a VKA in randomised trials, dabigatran 150 mg twice daily reduced the risk of stroke,20 dabigatran 110 mg twice daily reduced the rate of major bleeding,20 apixaban reduced the rate of mortality, stroke and major bleeding,21 and all three agents were associated with a lower rate of intracerebral haemorrhage.21–23 Furthermore, their use has practical advantages, which include fixed dosing, no need for blood test monitoring and fewer drug interactions when compared with warfarin.
erged as alternatives to warfarin for stroke prevention in patients with AF. When compared with a VKA in randomised trials, dabigatran 150 mg twice daily reduced the risk of stroke,20 dabigatran 110 mg twice daily reduced the rate of major bleeding,20 apixaban reduced the rate of mortality, stroke and major bleeding,21 and all three agents were associated with a lower rate of intracerebral haemorrhage.21–23 Furthermore, their use has practical advantages, which include fixed dosing, no need for blood test monitoring and fewer drug interactions when compared with warfarin.
These data form the evidence base for current clinical practice regarding stroke prevention in patients with AF. The balance between benefit and risk from OAC should be assessed through formal stratification of stroke risk using the CHA2DS2-VASc score (see Table 1) and the bleeding risk using the HAS-BLED score.24,25 Stroke risk is very low in men with a CHA2DS2-VASC score of 0 and in women with a CHA2DS2- VASc score of 1. A HAS-BLED score ≥3 is associated with an elevated risk of bleeding in patients taking OAC. Nevertheless, most patients with AF should be treated with OAC to lower their risk of stroke.24 Aspirin monotherapy is not recommended for the prevention of stroke in patients with AF.26 DAPT should only be considered for this purpose in patients who refuse to take OAC or in whom there is a clear contraindication to OAC and the bleeding risk is low.24
Antithrombotic Therapy Following Percutaneous Coronary Intervention for Patients with an Indication for Oral Anticoagulation
Nearly 10 % of patients who undergo PCI have an indication for longterm OAC.27 Coronary artery disease which requires PCI is present in more than 20 % of patients with AF.28 There are currently no definitive randomised trial data to guide decision-making regarding antithrombotic regimens following PCI for these patients. The inferior efficacy of OAC compared with DAPT for the prevention of stent thrombosis and the converse situation in relation to stroke prevention in patients with AF has led to the assumption that all three antithrombotic agents are required in order to achieve an acceptably low rate of adverse cardiac and cerebral events after PCI in patients who have AF.