Potential Future Antithrombotic Strategies with a Limited Evidence Base
Non-vitamin K Antagonist Oral Anticoagulant-based Antithrombotic Therapy
Dabigatran, apixaban and rivaroxaban were associated with significantly lower rates of intracranial haemorrhage than warfarin in randomised trials of stroke prevention in patients with AF,21–23 while dabigatran at a dose of 110 mg twice daily22 and apixaban also significantly reduced the rate of major bleeding compared with VKA.21 These data combined with the more predictable pharmacokinetic and pharmacodynamic profile of NOACs compared with VKAs raise the prospect of triple therapy or dual therapy (NOAC and clopidogrel) regimens, which carry a lower risk of bleeding than warfarin-containing regimens.
Insights into the risk of bleeding with NOAC-based triple therapy come from studies, which have investigated the combination of a NOAC with DAPT to reduce ischaemic cardiac events in patients following ACS. In the Anti-Xa Therapy to Lower Cardiovascular Events in Addition to Standard Therapy in Subjects with Acute Coronary Syndrome - Thrombolysis In Myocardial Infarction (ATLAS ACS 2-TIMI 51) study, the addition of low dose rivaroxaban (either 2.5 mg or 5 mg twice daily) to DAPT reduced the composite endpoint of cardiac death, MI and stroke after ACS but increased the rate of major bleeding and of intracranial bleeding.39 The ATLAS ACS 2-TIMI 46 study was designed to assess the safety and efficacy of various doses of rivaroxaban in combination with DAPT after ACS. In this study, the combination of DAPT with rivaroxaban 20 mg daily, its usual dose for stroke prevention in AF, rates of TIMI major and TIMI minor bleeding within six months were low at 1.8 and 0.9 %, respectively, but the rate of bleeding requiring medical attention at 180 days was 14.3 %.40 In the Randomized Evaluation of Long-Term Anticoagulation Therapy (RELY) study, which defined the relative efficacy and safety of dabigatran 110 mg twice daily, dabigatran 150 mg twice daily and warfarin for stroke prevention in AF, 38 % of the 18,113 patients also received antiplatelet therapy during the study period. The rate of bleeding was significantly higher in patients who took OAC plus one antiplatelet agent than in patients who took OAC only and was highest in patients who took OAC and DAPT irrespective of the OAC used. However, the rate of bleeding was lowest for patients who took dabigatran 110 mg twice daily, whether they were taking OAC only, OAC plus one antiplatelet agent or OAC plus DAPT.41 NOAC-based triple therapy has not yet been compared with warfarin-based triple therapy in a randomised trial. Further research is needed to define whether or not NOAC or warfarin is the preferred OAC for patients who require OAC following PCI.
Antithrombotic Combination Therapy Incorporating New Antiplatelet Agents
About 20 % of patients who undergo PCI achieve inadequate inhibition of platelet function from clopidogrel therapy.42 These clopidogrel non-responders experience higher rates of cardiovascular events than clopidogrel responders. Prasugrel and ticagrelor are newer, more potent antiplatelet agents than clopidogrel, which are being used with increasing frequency after ACS.
Prasugrel is a potent thienopyridine, which has less inter-individual variation in platelet inhibition than clopidogrel. In the Trial to Assess Improvements in Therapeutic Outcomes by Optimizing Platelet Inhibition with Prasugrel - Thrombolysis In Myocardial Infarction 38 (TRITON-TIMI 38), prasugrel and aspirin was superior to clopidogrel and aspirin in reducing adverse cardiac events (primarily MI and stent thrombosis) following an ACS.43 The increased efficacy of prasugrel came at the expense of significantly increased rates of major bleeding, including life-threatening bleeding. In the only published registry of patients taking triple therapy comprising aspirin, prasugrel and warfarin (used in 21 patients), this regimen was associated with a more than fourfold increase in bleeding (28.6 versus 6.7 %; p<0.001) without any difference in efficacy when compared with aspirin, clopidogrel and warfarin (taken in 356 patients).44
Ticagrelor is a direct-acting, reversible inhibitor of the platelet P2Y12 receptor. Like prasugrel, it provides more consistent inhibition of platelet function than clopidogrel. In the Study of Platelet Inhibition and Patient Outcomes (PLATO), patients with ACS who were randomly allocated to receive the combination of ticagrelor and aspirin experienced lower rates of recurrent MI and of all-cause mortality than patients who were randomly allocated to receive clopidogrel and aspirin.45 There was no significant difference in rates of major bleeding between the ticagrelor and cl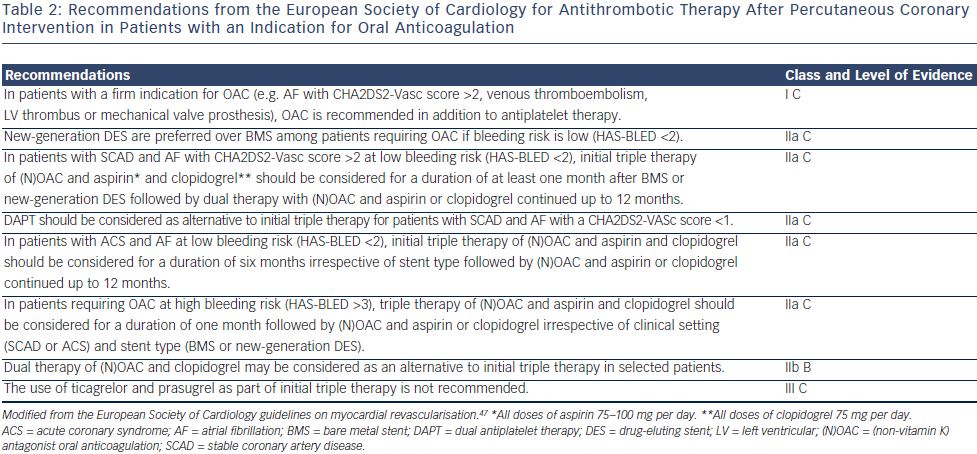 opidogrel groups (11.6 versus 11.2 %, respectively; p=0.4). There are currently no data, which describe the efficacy and safety of ticagrelor-based triple therapy. In PLATO, for instance, the study medication was stopped if OAC was administered. However, a recently published small Swedish study described outcomes among 107 patients with ACS who were discharged taking a combination of ticagrelor and warfarin and compared them to a historical control group of 159 patients with a similar baseline bleeding risk who were discharged taking aspirin, clopidogrel and warfarin.46 Rates of major bleeding and of ischaemic events (a composite of stroke or TIA, arterial embolism and recurrent ACS) at three months were not significantly different (7.5 versus 7.0 % and 4.7 versus 3.2 %, respectively) in patients taking ticagrelor and warfarin compared with triple therapy. Further data are required before firm recommendations can be made regarding combinations of antithrombotic therapy, which include OAC and prasugrel or ticagrelor.
opidogrel groups (11.6 versus 11.2 %, respectively; p=0.4). There are currently no data, which describe the efficacy and safety of ticagrelor-based triple therapy. In PLATO, for instance, the study medication was stopped if OAC was administered. However, a recently published small Swedish study described outcomes among 107 patients with ACS who were discharged taking a combination of ticagrelor and warfarin and compared them to a historical control group of 159 patients with a similar baseline bleeding risk who were discharged taking aspirin, clopidogrel and warfarin.46 Rates of major bleeding and of ischaemic events (a composite of stroke or TIA, arterial embolism and recurrent ACS) at three months were not significantly different (7.5 versus 7.0 % and 4.7 versus 3.2 %, respectively) in patients taking ticagrelor and warfarin compared with triple therapy. Further data are required before firm recommendations can be made regarding combinations of antithrombotic therapy, which include OAC and prasugrel or ticagrelor.
Current Guidelines
The use of triple therapy in patients after PCI is determined by the strength of their indication for OAC. The 2014 European Society of Cardiology/European Association for Cardio-Thoracic Surgery guidelines on myocardial revascularisation recommend that triple therapy should be used in patients with AF who have a CHA2DS2-VASc score >2, mechanical heart valves, intracardiac thrombus or recent or recurrent venous thromboembolism (see Table 2).47 They recommend that decisions regarding stent type (DES or BMS) and duration of triple therapy are made after formal assessment of the bleeding risk using the HAS-BLED score. Patients who are at low risk of bleeding (HAS-BLED score ≤2) should be treated using new-generation DES in preference to BMS, since these patients are likely to tolerate a longer period of triple therapy than other patients. By contrast, it is recommended that the duration of triple therapy should not exceed one month in patients who have a high bleeding risk (HAS-BLED score >3). In these patients, the choice of stent (DES or BMS) should be decided on an individual basis, and OAC and clopidogrel may be considered as an alternative to triple therapy.