Percutaneous coronary intervention (PCI) is one of the most commonly performed procedures in cardiology. More recently, the limitations of rigid metallic stents have led to the development of bioresorbable scaffolds (BRS). The earliest version of bioresorbable stent developed and tested in humans in 1990 was the Igaki-Tamai stent. It featured a thermal and balloon expandable stent that showed good outcomes at six months1 as well as long-term2 with neointimal hyperplasia similar to bare metal stents (BMS). The use of heat expansion, however, limited the clinical applicability of this device due to concerns of arterial wall necrosis with consequential platelet adhesion and stent thrombosis (ST).3 The development of new generation of BRS with improving mechanical performance is believed by some to be the next evolutionary leap in interventional cardiology. The major objective of this article is to review the evidence on BRS and identify their clinical applicability in current interventional practice.
Problems With Metallic Stents and the Benefits of Bioresorbable Scaffolds
In earlier days of balloon angioplasty, the adverse coronary vessel remodelling secondary to neointimal proliferation and extracellular matrix deposition as well as vessel recoil led to high restenosis rates.4,5 This early luminal loss was largely overcome by development of BMS that avoided vessel recoil and constrictive effects of vessel remodelling as well as any coronary flow impairment due to local dissections.6,7 However, the neointimal proliferative reaction to foreign body (metallic stent) resulted in greater intimal proliferation.8 The volume of neointimal proliferation was improved by introduction of drug eluting stents (DES) with anti-proliferative agents bound to stent polymers.9 Despite extensive literature on reduced revascularisation rates with DES, there have been multiple reports and safety concerns regarding occurrence of late and very late ST with DES.10 It was thought to be due to delayed and at times incomplete endothelialisation. This was a result of chronic inflammation from hypersensitivity reaction to the metallic stent and/or the durable polymers, which attenuates vascular healing.11–13 The presence of drug elution and a metallic stent are also believed to interfere with endothelial function.14,15 In addition, the persistent metallic scaffolding would subsequently limit expansive remodelling of the coronary artery. Loss of cyclic strain relief and protruding stru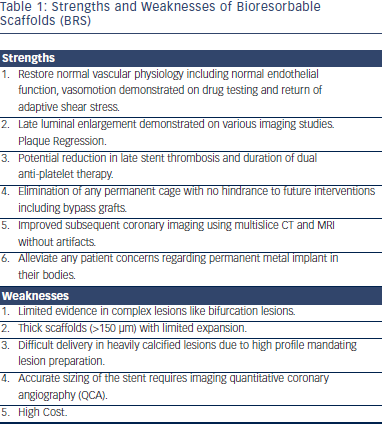 ts with resultant abnormal shear stress and strut fracture are other potential reasons for late cardiac events.
ts with resultant abnormal shear stress and strut fracture are other potential reasons for late cardiac events.
The primary notion of BRS was to facilitate complete vascular healing and restore normal endothelial function while providing equivalent mechanical properties of a metallic DES in the earlier stages (see Table 1). This was confirmed in recent imaging studies that demonstrated complete scaffold resorption and positive vessel remodelling. It was further accompanied by increase in luminal dimensions (plaque regression) and improved vasomotor function on drug (acetylcholine, nitroglycerin) testing.16 The incidence of late recurrence of residual anginal symptoms is high in patients who receive metallic DES; thus future trials are being designed to study the benefit of BRS in reducing residual angina symptoms.17
The complete disappearance of stent further appears attractive in plausibly eliminating the incidence of late and very-late ST. This could possibly shorten the duration of dual antiplatelet therapy (DAPT) and consequently reduce bleeding complications. The resorption of scaffolds would also plausibly avoid any hindrance from previous metal prosthesis during future interventions including placement of a bypass graft if needed in the future. Additionally, this could avoid problems associated with poorly aligned platforms or those blocking the side-branches.3 This is especially valuable in multivessel disease requiring multiple stent implantations. Indeed, > 100 mm of stent was implanted in the Synergy between PCI with taxus and cardiac surgery SYNTAX) trial in more than one-third of the enrolled patients.18 The DES are known to produce a “blooming artifact” on coronary computed tomography (CT) angiograms that could result in underestimation of intra-stent luminal diameter due to thickened appearance of the stent struts.19,20 The BRS without any metal would thus afford the benefit of allowing better subsequent coronary imaging using multislice computerised tomography (CT) and magnetic resonance imaging (MRI) without artifacts.21 Furthermore, BRS can be intuitively thought of as drug reservoirs for local delivery due to their modifiable resorption rates.3 Lastly, bioresorbable stents would eradicate any patient concerns regarding permanent metal implant in their bodies.22