Introduction and Objectives
A symposium, chaired by Dr Heinz Joachim Büttner of Freiburg-Bad Krozingen (Germany) and Dr Masahisa Yamane of St Luke’s International Hospital (Tokyo, Japan) took place at EuroPCR, Paris on May 23rd, 2014. Its objectives were as follows: to learn how to improve the success of percutaneous intervention (PCI) in chronic total occlusion (CTO) by matching techniques to anatomical and clinical characteristics; to improve procedural skills in CTO and complex PCI by sharing experience with established operators during transmitted live cases; to understand why bioabsorbable polymer or po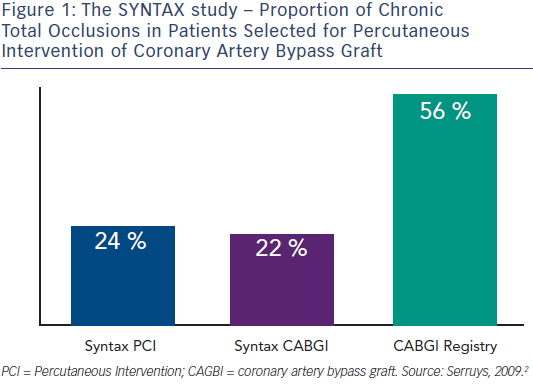 lymer-free sirolimuseluting stents can improve long-term benefit in patients undergoing complex and CTO PCI and how to use imaging modalities to facilitate CTO recanalisation.
lymer-free sirolimuseluting stents can improve long-term benefit in patients undergoing complex and CTO PCI and how to use imaging modalities to facilitate CTO recanalisation.
Chronic total occlusions remain the most challenging lesions treated by interventional cardiologists. Approximately 30 % of all coronary angiograms in patients with coronary artery disease (CAD) show a CTO.1 These represent around 24 % of the patient population treated by PCI and 22 % of those treated by coronary artery bypass graft (CABG) according to the Synergy between PCI with Taxus™ and cardiac surgery (SYNTAX) study. The majority of patients with CTO (56 %) are denied PCI and sent to surgery (see Figure 1).2 Successful recanalisation of a CTO is a strong independent predictor for reduced long-term mortality in patients with three vessel disease (3VD) but not with 1+2VD.3 In patients with multi-vessel disease and ST-elevation myocardial infarction (STEMI) undergoing primary PCI in the Harmonising outcomes with revascularisation and stents in acute myocardial infarction (HORIZONS-AMI) trial, a CTO in a non -infarctrelated artery was an independent predictor of early mortality. The presence of a CTO in a non-IRA was also an independent predictor of increased late mortality u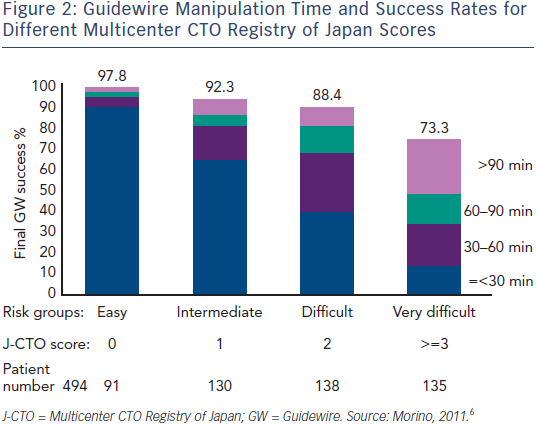 p to three years.4 A meta-analysis of randomised clinical trials and observational studies suggested that complete revascularisation is the optimal strategy in both CABG and PCI in patients with multi-vessel disease.5
p to three years.4 A meta-analysis of randomised clinical trials and observational studies suggested that complete revascularisation is the optimal strategy in both CABG and PCI in patients with multi-vessel disease.5
Despite the improving success rates of PCI in CTO, they are still inferior compared to non-occlusive CAD. There is a great diversity in the complexity of the CTO lesion and the J-CTO (Multicenter CTO Registry of Japan) score has been developed as a model to stratify the complexity and predict expected success rates. According to that model there are four difficulty groups: easy (J-CTO score of 0), intermediate (score of 1), difficult (score of 2) and very difficult (score of ≥ 3), (see Figure 2).6 Score points were determined by assigning one point in the presence and zero in the absence of each of the following angiographic characteristics: calcification, intra CTO bending, blunt stump, occlusion length >20 mm and a previously failed lesion. Guidewire manipulation time and success rates for different J-CTO scores are shown in Figure 2.
Recanalisation techniques include the anterograde (single wire, parallel wire, intravascular ultrasound [IVUS] navigated, and their variations), the retrograde that require collateral crossing, CTO entering, wire (re)entry beyond CTO via reverse CART (controlled antegrade and retrograde tracking (CART), direct wire crossing kissing wire and their variations, and the dissection re-entry techniques that they can be used both antegrade and retrograde.
The publication of the article was supported by Alvimedica.