Migraine
The link between PFO and migraine, particularly with aura, was initially suggested in the late 1990s,31–33 and in non-randomised retrospective analyses up to 80 % of patients who underwent PFO closure for alternative indications reported an improvement or even cessation of migraine. Wilmshurst et al.34 contacted 37 patients who had undergone closure of a right to left shunt of whom 21 (57 %) had a history of migraine before the procedure (with aura in 16, without in five). During long-term follow-up, ten patients reported no further migraine symptoms with a further eight others reporting improvement in frequency and severity of migraines. A single-centre, non-randomised trial of PFO closure in the context of migraine in patients with high-risk (for PE) anatomy found a significant reduction in migraine in the device closed patients.35
MIST Trial
The Migraine Intervention with STARFlex Technology (MIST) trial36 is the only published randomised trial addressing the question of PFO closure in the context of migraine, and did not meet its primary endpoint (complete freedom from headache) or si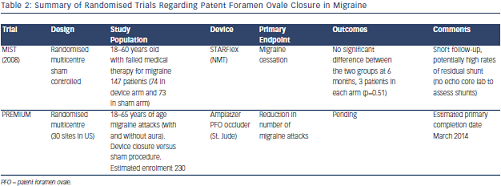 gnificantly reduce headache burden. Follow-up was short (six months) and the inclusion criteria may have selected refractory headache patients. The lack of an independent core echocardiography laboratory has led to controversy about the effectiveness of closure, and procedural complications were high at 6.8 %, which may have influenced the outcome of the study.
gnificantly reduce headache burden. Follow-up was short (six months) and the inclusion criteria may have selected refractory headache patients. The lack of an independent core echocardiography laboratory has led to controversy about the effectiveness of closure, and procedural complications were high at 6.8 %, which may have influenced the outcome of the study.
The Prospective Randomized Investigation to Evaluate Incidence of Headache Reduction in Subjects With Migraine and PFO Using the Amplatzer PFO Occluder to Medical Management (PREMIUM) trial with a primary endpoint of reduced migraine attacks has finished recruiting and expects to release results in the next 12 months, and although now terminated, data may be available from the international Percutaneous Closure of Patent Foramen Ovale In Migraine With Aura (PRIMA) trial in due course. Studies summarised in Table 2.
Platypnoea-orthodeoxia Syndrome
In patients with POS, significant right to left shunting occurs dependent upon position leading to desaturation on sitting or standing. In the context of PFO this can occur in any situation where atrial septal geometry is modified or heart-lung relationships are altered. Examples of such situations are kyphoscoliosis, post-pneumonectomy, diaphragm paralysis and dilatation of the ascending aorta.
The first reported case of PFO closure for POS, performed surgically in 1991, was in a patient with PFO and idiopathic hemidiaphragm paralysis.37 Subsequently device closure in similar patients has been shown to eliminate hypoxia38 and although rare, this clearly should be considered in all patients with restricting symptoms.39
Diving and Decompression Illness
PFO has been associated with specific presentations of decompression illness in divers;40,41 studies have been performed to identify those at higher risk42 and closure following neurological decompression illness has been reported.43 PFO closure in continuing divers appears to prevent symptomatic neurological events and asymptomatic ischaemic brain lesions during long-term follow-up,44 and has been shown to reduce arterial, although not venous, bubbles in simulated dives.45
Neither recreational nor professional bodies recommend PFO screening in divers unless there has been an episode of a potentially PFO-attributable decompression illness. Given the complexity of assessing this, review by a physician with specific knowledge of diving medicine is mandatory. Recreational divers can be advised to restrict themselves to shallow depths (usually less than 15 m) and to adopt techniques to reduce nitrogen super-saturation including diving with nitrox using air tables and avoiding repetitive dives, or to consider PFO closure.46 Professional divers will require sign-off by a diving specialist and this often includes removal of a shunt if clinically relevant to avoid disabling employment restrictions.30
Surgery in the Seated Position
Some neurosurgery is preferably performed in the seated position and paradoxical air embolism is a well-recognised hazard. Perkins-Pearson et al.47 demonstrated reversal of the normal inter-atrial pressure gradient making patients with an atrial communication at risk of PE, and therefore the presence of a PFO is generally regarded as an absolute contraindication to surgery in the seated position. There are cases of PFO closure performed in this setting;48 however, there are no large studies and there remain questions about the timing of surgery post-intervention, with regard to endothelialisation of the device and duration of antiplatelet therapy.