Acute and Long-term Clinical Outcome After Driver-guided Ablation
In our series of 103 persistent AF patients who underwent driverbased ablation,14 AF terminated during the procedure in 82 (80 %) patients with RF duration of 35±21 minutes. The mode of termination was SR in 28 (34 %) and AT in 54 (66 %) patients. AF termination with only driver ablation without linear lesions was achieved in 65 (63 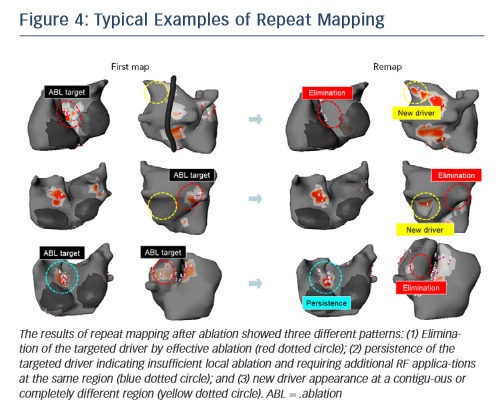 %) patients. The number of targeted region for AF termination increased with AF duration (three in AF lasting <3 months, four in AF lasting 4–6 months and six in AF lasting >6 months). Inversely, the termination rate decreased with AF duration (85 % in AF lasting <3 months, 82 % in AF lasting 4–6 months, 67 % in AF lasting 7–9 months, 36 % in AF lasting 10–12 months and 15 % in AF lasting >12 months). Moreover, the patients with SR at the beginning of the procedure demonstrated the highest termination rate of 88 %. An impressive finding of driverbased ablation is that high AF-termination rate was achieved with re-duced RF-time compared with the stepwise approach (28±17 versus 65±33; p<0.0001). At 12 months post ablation, 64 % of patients maintained SR and 22 % were in AT. In this study, 85 % patients with AF termination were free from AF at 1 year after the procedure, which was comparable to stepwise ablation strategy. Also, the AF-free survival rate was higher in patients with acute AF termination than non-termination (85 % versus 63 %; p=0.045). In another population, RF time for AF termination increased with the number of driver regions and correlated to cycle length of left and right atrial appendages (see Figure 2B).39 Continuous AF duration, left appendage cycle length, number of reentrant drives and surface area of LA were independent predictors of AF termination on multivariable analysis (see Figure 2C). These results suggest that driver-based ablation is feasible and effective in patients with persistent AF and those having progressed atrial remodelling with extended fibrosis (AF duration >12 months) continue to pose a challenge.
%) patients. The number of targeted region for AF termination increased with AF duration (three in AF lasting <3 months, four in AF lasting 4–6 months and six in AF lasting >6 months). Inversely, the termination rate decreased with AF duration (85 % in AF lasting <3 months, 82 % in AF lasting 4–6 months, 67 % in AF lasting 7–9 months, 36 % in AF lasting 10–12 months and 15 % in AF lasting >12 months). Moreover, the patients with SR at the beginning of the procedure demonstrated the highest termination rate of 88 %. An impressive finding of driverbased ablation is that high AF-termination rate was achieved with re-duced RF-time compared with the stepwise approach (28±17 versus 65±33; p<0.0001). At 12 months post ablation, 64 % of patients maintained SR and 22 % were in AT. In this study, 85 % patients with AF termination were free from AF at 1 year after the procedure, which was comparable to stepwise ablation strategy. Also, the AF-free survival rate was higher in patients with acute AF termination than non-termination (85 % versus 63 %; p=0.045). In another population, RF time for AF termination increased with the number of driver regions and correlated to cycle length of left and right atrial appendages (see Figure 2B).39 Continuous AF duration, left appendage cycle length, number of reentrant drives and surface area of LA were independent predictors of AF termination on multivariable analysis (see Figure 2C). These results suggest that driver-based ablation is feasible and effective in patients with persistent AF and those having progressed atrial remodelling with extended fibrosis (AF duration >12 months) continue to pose a challenge.
Recently, a prospective multicentre study (non-invasive mapping of atrial fibrillation study [AFACART]) demonstrated feasibility and utility of body surface mapping in persistent AF.40 In this study, 118 persistent AF patients (AF duration <1 year) were enrolled among eight European centres that had no prior experience using noninvasive system for driver-guided ablation to evaluate its acute success rate, RF time and clinical outcome at 12 months. Acute success (AF termination) was achieved in 64 % patients by driverbased ablation with 46±28 minutes of RF time. During 6±3 months’ follow-up, 83 % of patients were free from AF including recurrent AT in 38 % patients. These results indicate that driver-guided ablation of persistent AF is feasible and its outcomes reproducible in centres with no prior experience.
Limitation and Prospects of Body Surface Mapping
Non-invasive body surface mapping of AF drivers have some limitations: 1) Assessment of the drivers in the septal area is difficult. It is projected posteriorly on right atrium or anteriorly in the interatrial groove from right/left septum. These areas are close to each other and located under the epicardium making it difficult to identify driver area from body surface signals. 2) Agreement between driver areas and ablation sites may not be perfect because the body surface mapping system (ECVUE) does not have 3D-mapping navigation system. Although image integration with CARTO3 is possible, it may not be performed in all cases. 3) Accuracy of detection of small amplitude and very short cycle length (very rapid drivers) signals is not reliable because of the preset limits on the range of acceptable signal/noise ratio and window of analysable AF cycle length (4–8 Hz). The sensitivity is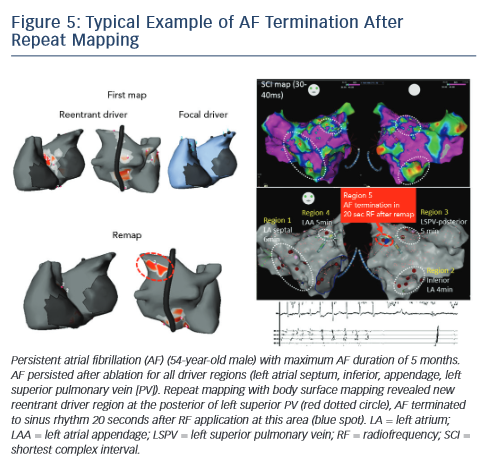 low in the case of far-field and small signals (<0.15 mV), particularly in scar tissue where they may not be detected correctly. In such areas, global activation can be used as a surrogate, yet it may be difficult to distinguish reentrant activity from focal activity. 4) Reconstructed epicardial electrogram signals may be affected by tissues between the epicardium and body surface and specific anatomical conditions (high/low BMI, lung disease, limited coverage of the vest due to body habitus). 5) Transformation of data to phase-based analysis may demonstrate false reentrant activity because of interpolation of incomplete wave curvatures. To resolve this matter, local raw electrograms need to be checked manually to ascertain sequential propagation of regional waves. 6) Finally, reentrant and focal drivers detected by non-invasive body surface mapping were not validated by concurrent endocardial mapping, AF substrates are dynamic 3D structures with a range of discordance between the endocardial and epicardial tissue.41 Hence further examinations will be needed to validate AF mechanisms including reentrant and focal drivers.
low in the case of far-field and small signals (<0.15 mV), particularly in scar tissue where they may not be detected correctly. In such areas, global activation can be used as a surrogate, yet it may be difficult to distinguish reentrant activity from focal activity. 4) Reconstructed epicardial electrogram signals may be affected by tissues between the epicardium and body surface and specific anatomical conditions (high/low BMI, lung disease, limited coverage of the vest due to body habitus). 5) Transformation of data to phase-based analysis may demonstrate false reentrant activity because of interpolation of incomplete wave curvatures. To resolve this matter, local raw electrograms need to be checked manually to ascertain sequential propagation of regional waves. 6) Finally, reentrant and focal drivers detected by non-invasive body surface mapping were not validated by concurrent endocardial mapping, AF substrates are dynamic 3D structures with a range of discordance between the endocardial and epicardial tissue.41 Hence further examinations will be needed to validate AF mechanisms including reentrant and focal drivers.
The non-invasive technique has been recently used to remap AF immediately after driver ablation. In fact, the critical point of driverbased ablation is to assess elimination of drivers after ablation. Moreover, incomplete RF application may not impact drivers or generate new AF substrate via slow conduction in the heterogenous region. In a small number of patients, we have shown the results of repeat mapping with different patterns (elimination, persistence and new appearance of driver) (see Figure 4).42 Figure 5 demonstrates a typical example of AF termination after repeat body surface mapping. A new reentrant driver appeared at the posterior of left superior PV on remapping AF persisting post driver ablation, AF was terminated by ablation in this area. Repeat non-invasive mapping provides important information on the dynamics of driver domains during ablation. Repeat mapping can reveal residual and new drivers, which have the potential to increase the AF termination rate and improve clinical outcomes.