Ischaemic Cardiomyopathy
There have been only three major prospective randomised clinical trials examining long-term outcomes after VT ablation in patients with ICM.14–16
The first large-scale prospective randomised controlled trial examining ablation versus medical therapy in patients with ICM was the Substrate Mapping and Ablation in Sinus Rhythm to Halt 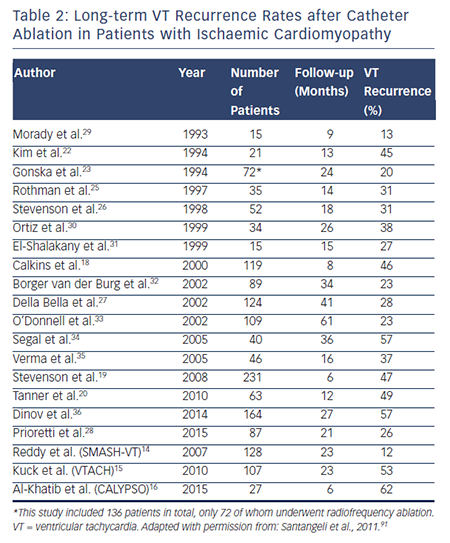 Ventricular Tachycardia (SMASH-VT) study.14 This trial initially enrolled only patients with recently implanted ICDs for secondary prevention and later included those who underwent ICD implantation for primary prevention who had received an appropriate ICD therapy for a single VT or ventricular fibrillation (VF) episode. A total of 128 patients were enrolled and randomly assigned to catheter ablation or medical therapy (64 in each arm). The primary endpoint was survival from any appropriate ICD therapy (ATP or shock), and secondary endpoints included freedom from inappropriate ICD shock, death and ICD storm (≥3 shocks in 24-hour period). Freedom from recurrent VT/VF resulting in appropriate ICD therapy after 2 years of follow-up was significantly higher in the ablation arm (88 versus 67 %; HR 0.35; 95 % CI 0.15–0.78; p=0.007) compared with controls.14
Ventricular Tachycardia (SMASH-VT) study.14 This trial initially enrolled only patients with recently implanted ICDs for secondary prevention and later included those who underwent ICD implantation for primary prevention who had received an appropriate ICD therapy for a single VT or ventricular fibrillation (VF) episode. A total of 128 patients were enrolled and randomly assigned to catheter ablation or medical therapy (64 in each arm). The primary endpoint was survival from any appropriate ICD therapy (ATP or shock), and secondary endpoints included freedom from inappropriate ICD shock, death and ICD storm (≥3 shocks in 24-hour period). Freedom from recurrent VT/VF resulting in appropriate ICD therapy after 2 years of follow-up was significantly higher in the ablation arm (88 versus 67 %; HR 0.35; 95 % CI 0.15–0.78; p=0.007) compared with controls.14
The second landmark trial was the Ventricular Tachycardia Ablation in Coronary Heart Disease (VTACH) study: a prospective, open, randomised control trial involving 16 centres in four European countries.15 The investigators enrolled 110 patients with haemodynamically stable VT, prior MI and reduced left ventricular ejection fraction (LVEF), who were randomly assigned to catheter ablation and ICD versus ICD alone. The primary endpoint was time to first VT/VF recurrence. Of the 107 patients included in the analysis (52 ablation; 55 control), median time to VT/VF recurrence in the ablation group was longer than the control group (18.6 versus 5.9 months). After 2 years, those randomised to ablation had superior VT/VF-free survival (47 versus 29 %; HR 0.61; 95 % CI 0.37–0.99; p=0.045) and were more likely to be free from cardiac hospital readmission (67 versus 45 %; HR 0.55; 95 % CI 0.30–0.99; p=0.044). Additionally, those in the ablation group on average had significantly fewer appropriate ICD shocks per patient year (mean 0.6±2.1 versus 3.4±9.2 shocks; p=0.018).15
The Catheter Ablation for VT in Patients with Implantable Cardioverter Defibrillator (CALYPSO) trial was a small prospective randomised trial comparing a strategy of early catheter ablation versus AADs for VT in patients with ICM with ICDs who had received appropriate ICD therapies for VT.16 This multicentre pilot study enrolled a total of 27 patients (13 ablation; 14 AAD), only 17 (71 %) of whom completed 6 months of follow-up. Rates of VT recurrence in this population of patients with multiple prior appropriate ICD therapies were significantly higher than those previously reported in SMASH-VT and VTACH: 62 % had recurrent VT in the ablation arm at 6 months following the ablation procedure.16
The 2-year VT-free survival rates in SMASH-VT and VTACH were 88 % and 47 %, respectively, while the 6-month VT-free survival rate in the much smaller CALYPSO trial was significantly lower (38 %), probably due to the fact that the trial selectively enrolled higher-risk patients known to have recurrent VT requiring appropriate ICD therapies.
Prospective non-randomised studies examining patients with ICM and varying VT burden have reported a wide range of long-term VT-free survival following ablation.
In 1997, Strickberger et a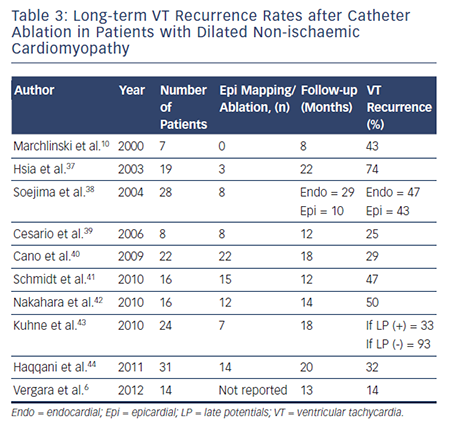 l. prospectively enrolled 21 patients with ICD and frequent ICD therapies (mean of 25±88 ICD therapies within 36±51 days preceding ablation). Acute abolition of the clinical VT occurred in 76 %.17 Although this study did not report overall long-term VT-free survival, they did report a decrease in frequency of ICD therapies and improvement in quality of life in those with acute ablation success over a follow-up period of 11.8±10 months.17
l. prospectively enrolled 21 patients with ICD and frequent ICD therapies (mean of 25±88 ICD therapies within 36±51 days preceding ablation). Acute abolition of the clinical VT occurred in 76 %.17 Although this study did not report overall long-term VT-free survival, they did report a decrease in frequency of ICD therapies and improvement in quality of life in those with acute ablation success over a follow-up period of 11.8±10 months.17
The Cooled RF Ablation System clinical trial (2000) was a prospective, observational trial that included 146 patients with SHD, the majority (82 %) of whom had ICM.18 All patients had ICD implanted with haemodynamically stable VT and had failed at least two AADs. Mean follow-up duration was 243±153 days. One year after ablation, the VT recurrence rate was 56 %, while the 1-year mortality rate was 25 %. Of the 122 patients with at least 2 months clinical follow-up, 81 % had >75 % reduction in VT frequency in the first 2 months after ablation. The Multicenter Thermocool VT Ablation Trial was a prospective observational trial that enrolled 231 patients with recurrent monomorphic VT in setting of ICM treated with catheter ablation.19 This study was focused on evaluating the efficacy of VT ablation in very high-risk patients, and therefore included patients with haemodynamically unstable, unmappable and multiple VTs. After 6 months, 53 % of patients were free from recurrent incessant VT or intermittent VT and the mortality rate at 1 year was 18 %.19
The EURO-VT study was a multicentre, prospective, non-randomised observational study that enrolled 63 ICM patients with multiple (>4) episodes of symptomatic VT within 6 months (or VT storm) of randomisation.20 Over mean follow-up of 12 months, 49 % had VT recurrence, although the majority (79 %) of those with VT recurrence had reduction in ICD therapies.20
Retrospective observational studies examining VT ablation for patients with ICM published have reported varying long-term rates of VT recurrence ranging from 16 to 66 %. Table 2 summarises long-term outcomes of VT ablation in patients with ICM.10,14–16,18–36
Non-ischaemic Cardiomyopathy
To date, there have been no prospective randomised trials describing outcomes following VT ablation in patients with NICM. Patients with NICM have higher rates of acute procedural failure and long-term VT recurrence following ablation compared with ICM.28,36 Unlike ICM, 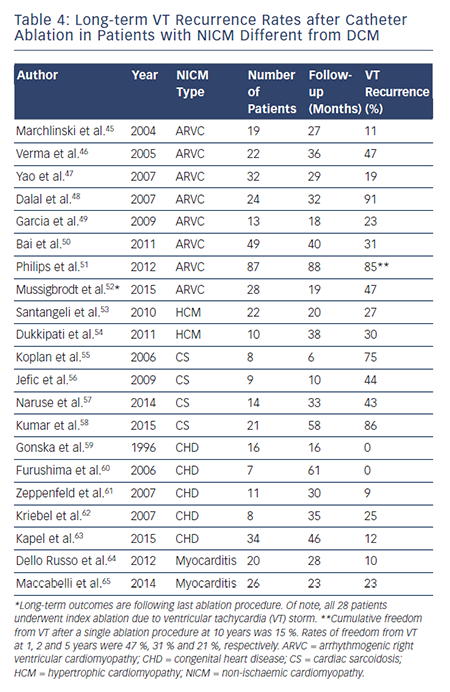 where the underlying substrate is relatively homogeneous, patients with NICM have heterogeneous substrates that reflect the variety of pathogenetic processes. However, the distribution of abnormal substrates in patients with non-ischaemic pathology has been shown fairly homogeneous, with a typical involvement of perivalvular regions and high prevalence of intramural and/or epicardial substrates. Table 3 summarises long-term outcomes of VT ablation in dilated NICM (DCM),6,10,37–44 and Table 4 summarises long-term outcomes of VT ablation in other forms of NICM.45–65
where the underlying substrate is relatively homogeneous, patients with NICM have heterogeneous substrates that reflect the variety of pathogenetic processes. However, the distribution of abnormal substrates in patients with non-ischaemic pathology has been shown fairly homogeneous, with a typical involvement of perivalvular regions and high prevalence of intramural and/or epicardial substrates. Table 3 summarises long-term outcomes of VT ablation in dilated NICM (DCM),6,10,37–44 and Table 4 summarises long-term outcomes of VT ablation in other forms of NICM.45–65
The Heart Center of Leipzig VT (HELP-VT) study was a prospective observational European single-centre study that enrolled 63 patients with NICM and 164 patients with ICM who were treated with VT ablation between 2008 and 2011.36 Activation mapping and ablation were performed in nearly half of patients, and substrate modification was not uniformly performed. Acute procedural success (defined as complete non-inducibility after ablation) was achieved in 66.7 % of those with NICM (versus 77.4 % in ICM; p=0.125). Long-term VT-free survival was significantly lower for NICM compared with ICM: cumulative VT-free survival after median follow-up periods of 20 and 27 months for NICM and ICM, respectively, were 23 % and 43 % (HR 1.62, 95 % CI 1.12–2.34; p=0.01). VT-free survival rates at 1 year were 40.5 % for NICM and 57 % for ICM.36
Proietti et al. recently reported their experience with a substrate-guided ablation approach in 55 NICM and 87 ICM patients.28 They showed lower rates of freedom from recurrent VT in those with NICM compared with ICM (49 % versus 74 %; p=0.03) over a follow-up period of 21.1 months. They attributed their higher rates of long-term success (compared with previous reports) to the fact that higher rates of acute procedural success might have been achieved using a substrate-based approach.28
One large single-centre retrospective observational study, which examined 226 patients with NICM treated with VT ablation, reported 29 % rate of death or transplant at long-term follow-up (4.4±3.3 years follow-up), while the secondary composite endpoint of death, heart transplantation or hospitalisation for VT recurrence at 1 year (after the last ablation) was 31 %.66
Dilated Cardiomyopathy
Patients with DCM tend to have worse prognosis after VT ablation compared with arrhythmogenic right ventricular cardiomyopathy (ARVC) and congenital heart disease (CHD).66 Retrospective studies have demonstrated VT recurrence rates ranging between 46 and 61 % during long-term follow-up (mean 11–25 months for individual studies).38
Patterns of scar in non-ischaemic DCM have been previously described. Classically, there is involvement of the base of the heart along the perivalvular region, particularly around the basolateral LV.37,67 In this group of patients, the prevalence of intramural and epicardial substrates is high. At our institution, up to 11.3 % of all NICM patients had an isolated septal substrate. Haqqani et al. reported that this particular population frequently required multiple procedures to achieve VT control. VT recurred in 32 % of patients over mean follow-up of 20 months after ablation.44 Oloriz et al. later classified 87 NICM patients treated with ablation as having either predominantly anteroseptal versus inferolateral scar based on endocardial unipolar voltage mapping.68 Patients with inferolateral scar frequently had epicardial substrate, while those with anteroseptal scar more often had intramural septal substrate. They noted a higher VT recurrence rate in those with anteroseptal scar (74 vs 25 %; p<0.001), resulting in higher redo ablation rate (59 versus 7 %; p<0.001). Anteroseptal scar was an independent predictor of VT recurrence in the multivariate analysis (HR 5.5; p<0.001).
Arrhythmogenic Right Ventricular Cardiomyopathy
Long-term success rates of VT ablation in patients with ARVC have historically been quite variable and highly dependent on the specific ablation approach adopted.45–48,52 Over a decade ago, Marchlinski et al. reported a long-term VT suppression rate of 89 % in 19 patients who underwent endocardial VT ablation over a mean follow-up duration of 27 months.45 They identified that in these patients, certain areas such as the perivalvular tricuspid/pulmonary valve regions and the RV free wall and septum (but not the RV apex) were more likely to harbour areas with abnormal electrograms. Verma et al. showed 1, 2, and 3-year VT recurrence rates of 23 %, 27 %, and 47 %, respectively.46 Dalal et al. later reported much worse long-term outcomes in 24 patients treated with endocardial VT ablation at 29 centres across the country between 1999 and 2006.48 In their study, they reported VT recurrence rates after a single procedure of 64 %, 75 %, and 91 % after 1, 2, and 3 years, respectively. They hypothesised that the dismal long-term success was due to the fact that ARVC was an electrically progressive disease.48 Later, Riley et al. elegantly showed with serial electroanatomical voltage mapping that although the RV progressively dilates, only the minority of patients have progression of endocardial scar, suggesting that an aggressive substrate modification may be effective in long-term VT control.69
In fact, given the more extensive epicardial pathological substrate in ARVC, catheter ablation approaches using a combination of endoepicardial substrate based ablation have been recently shown to significantly improve VT-free survival at the short to mid-term followup. 49–51,70 Garcia et al. reported a series of 13 ARVC patients with VT undergoing endo-epicardial mapping and ablation.49 The authors confirmed a more extensive epicardial involvement in these patients, with a reported success rate of 77 % over a mean follow-up time of 18 months. Similar findings have been reported by Bai et al.50 in a multicentre series of 49 patients undergoing either endocardial-only ablation (n=23), or endo-epicardial ablation (n=26). After a follow-up of at least 3 years, VT-free survival achieved 52.2 % in the endocardial-only ablation group and 84.6 % in the endo-epicardial ablation group. Two other studies from different institutions across US and Europe have recently reported the same results.51,70 In conclusion, endo-epicardial ablation is significantly more effective that endocardial-only procedures in achieving VT-free survival in patients with ARVC, essentially due to the peculiar epicardial to endocardial progression of the disease.
Hypertrophic Cardiomyopathy
Malignant ventricular arrhythmias in patients with hypertrophic cardiomyopathy (HCM) stem from pathological myocardial fibrosis, disruption of cellular architecture and hypertrophied myocytes,71,72 which constitute the substrate for reentrant VTs. Studies evaluating the pattern of myocardial tissue scarring in HCM reported a high prevalence of mid-myocardial and epicardial fibrotic areas.73,74 Remarkably, in a small subset of patients in whom the disease evolves to the end-stage leading to aneurysm formation, a transmural scar can be detected.75,76 Until recently, the clinical experience with catheter ablation of VT was limited to patients with end-stage forms of the disease with apical aneurysms.76,77 Two recent studies have reported the feasibility and safety of VT ablation in larger series of patients with HCM also without apical aneurysms.53,54 In a multi-centre observational study, Santangeli et al. evaluated the role of VT ablation in a series of 22 patients with multiple episodes of drug-refractory VTs.53 In this study, an endo-epicardial ablation was required in 59 % of cases, and no major procedural complication was observed. After an average follow-up of 20 months, freedom from recurrent VT reached 73 %. In a subsequent study, Dukkipati et al. reported 10 patients with HCM-related monomorphic VT treated with combined endocardial and epicardial ablation.54 Epicardial scar was identified in 80 % of patients, endocardial scar in 60 % and no scar in 10 %. Five patients had stable inducible monomorphic VT and were treated with combined endocardial and epicardial ablation. Four underwent combined endocardial and epicardial ablation with a substrate-based approach based on sites of late/fractionated potentials with good pace maps. The final patient was non-inducible and had no endocardial or epicardial scar, so no ablation was performed. During mean long-term follow-up of mean 37.4±16.9 months, only three (30 %) patients had ICD shocks for recurrent VT (including the lone patient who was noninducible and had no electroanatomic scar).54