Physical Examination
Physical examination centres on haemodynamic evaluation and assessing for the clinical signs of congestion (see Figu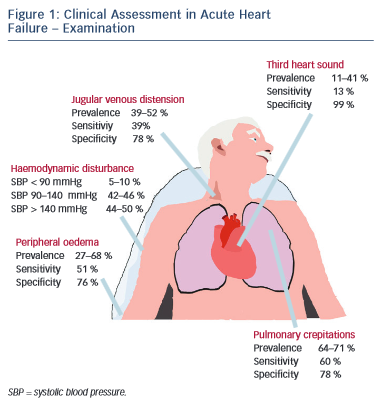 re 1). Patients with AHF may have a high, low or normal blood pressure. Normotension or moderate hypertension is the most common finding in observational series (see Table 2).2,3,18–21 Uncontrolled severe hypertension, particularly in conjunction with predominant pulmonary congestion may indicate hypertensive HF, HF with preserved EF (HF-PEF), or ‘flash’ pulmonary oedema in extreme cases. Hypotension (5–10 %) is the least-common manifestation but marks an important adverse prognostic sign, typically reflecting compromised cardiac output that, dependent on the patient, should prompt the consideration of either more advanced therapies, such as vasoactive agents and mechanical support, or the need for palliation.2,3,18–21 The temperature of the extremities as assessed by palpation may also used as an indicator of cardiac output. Cool peripheries are present in up to 24 % of unselected patients.19 The Forrester classification system based upon whether patients have adequate circulation (warm or cold) alongside the presence or absence of congestion (wet or dry) is no longer included in current guidelines but provides a useful guide to applied haemodynamics.29,30
re 1). Patients with AHF may have a high, low or normal blood pressure. Normotension or moderate hypertension is the most common finding in observational series (see Table 2).2,3,18–21 Uncontrolled severe hypertension, particularly in conjunction with predominant pulmonary congestion may indicate hypertensive HF, HF with preserved EF (HF-PEF), or ‘flash’ pulmonary oedema in extreme cases. Hypotension (5–10 %) is the least-common manifestation but marks an important adverse prognostic sign, typically reflecting compromised cardiac output that, dependent on the patient, should prompt the consideration of either more advanced therapies, such as vasoactive agents and mechanical support, or the need for palliation.2,3,18–21 The temperature of the extremities as assessed by palpation may also used as an indicator of cardiac output. Cool peripheries are present in up to 24 % of unselected patients.19 The Forrester classification system based upon whether patients have adequate circulation (warm or cold) alongside the presence or absence of congestion (wet or dry) is no longer included in current guidelines but provides a useful guide to applied haemodynamics.29,30
Assessment of the heart rate and rhythm will help to elicit important arrhythmias (e.g. atrial fibrillation), which may have triggered the presentation and will influence management. Other important ancillary signs, which indicate underlying structural heart disease, include cardiac murmurs. The most prevalent features of congestion are peripheral oedema (65–68 %) and bibasal crepitations or rales (64– 80 %), which in patients presenting to the emergency department with undifferentiated dyspnoea offer sensitivity and specificity of 51 and 76 % and 60 and 78 %, respectively.2,3,18–21
Measurement of the jugular venous pressure has been an integral part of bedside cardiology since its inception. In expert hands the value of jugular venous distension as an indicator of elevated right atrial pressure and its correlation with raised pulmonary capillary wedge pressure has been elegantly demonstrated in advanced chronic HF with excellent specificity.31,32 Yet even in this context the practical utility of this sign has not been universal, while in undifferentiated patients with acute dyspnoea sensitivity falls to as low as 39 %, perhaps reflecting in part a more general lack of confidence among the newer generation of clinicians in eliciting such signs.33–36 Similarly the third heart sound, a low pitched sound best heard over the left ventricular apex in conjunction with the rapid filing phase of ventricular diastole demonstrated excellent specificity and was an independent predictor of mortality in a large cohort of AHF patients in Japan.37 However, a lack of familiarity in the detection of this sign and poor inter-observer variability has been documented elsewhere, reflected in its low sensitivity (13–40 %) in patients with AHF presenting to the emergency department, even when augmented by acoustic cardiography (computerised measurement of the heart sounds with a synchronous electrocardiogram [ECG] trace using specialised electrodes placed at V3–V4).34,38–40
Special Considerations
Alongside an ageing population the demographics of HF patients are changing, e.g. changing cardiovascular risk profile (reduction in incidence of myocardial infarction) and developments in cardiac care (e.g. primary percutaneous coronary intervention). Some contemporary epidemiological series indicate the mean age at diagnosis may be as high as 80 years old.41 Patients in this category warrant special consideration and particular vigilance from the assessing clinician. Presentation may be subtle and more gradual, perhaps marked by atypical symptoms (e.g. anorexia and weight loss), with co-morbid conditions (e.g. musculoskeletal disease) acting as confounders to potentially decrease sensitivity.42 In contrast to their younger counterparts, elderly patients (>85 years) with AHF are more likely to be female and have a preserved EF.43 Atrial fibrillation, hypertension, anaemia, renal dysfunction and cerebrovascular disease are all more common – while diabetes and coronary artery disease are conversely less frequent – perhaps implying that patients with these conditions are more likely to present earlier.44 The expected typical examination findings are also less frequent compared with younger (<65 years of age) patients.45
The studies detailed above mostly refer to patients in Western Europe and the US. Outside of this demographic some main differences in the background and presentation of patients with AHF exist. In Eastern Europe, Asia, Africa and the Middle East, patients are much more likely to present acutely with de novo HF.46–50 Patients in Saudi Arabia are younger, with a higher incidence of diabetes and a greater preponderance for left ventricular systolic dysfunction.50 Patients in the Asian-Pacific are also younger, less co-morbid and tend to exhibit a more severe phenotype.49 Finally, across a range of sub-Saharan African countries the incidence of ischaemic heart disease is much lower than in western populations with hypertension the predominant HF aetiology.48
Chest Radiograph
The chest radiograph is a low cost, easily obtainable investigation that should be routine in all acutely dyspnoeic patients with suspected HF; serving to exclude alternative pathologies (e.g. pneumonia, pneumothorax, lung cancer) and/or demonstrate features of HF.13,14 The classic radiographic features of HF have been elegantly described in conjunction with physiological haemodynamic data and are detailed in Table 3.51,52 Pul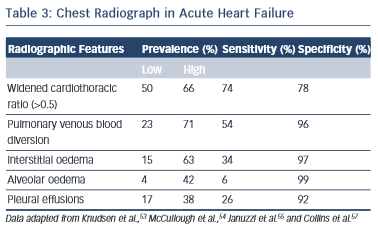 monary venous blood diversion (PVBD), or cephalisation, results from redistribution of the pulmonary blood flow and typically occurs when pulmonary artery wedge pressure (PAWP) is greater than 10–15 mmHg. Interstitial oedema, characterised by peripheral septal (Kerley B) lines due to thickening of the interlobular septa, is thought to result in a PAWP greater than 20 mmHg, while alveolar oedema is present when PAWP exceeds 25 mmHg.52 However, this hierarchy of radiographic changes is not ubiquitous and may only be partially present, or indeed absent, even in cases of advanced HF.51
monary venous blood diversion (PVBD), or cephalisation, results from redistribution of the pulmonary blood flow and typically occurs when pulmonary artery wedge pressure (PAWP) is greater than 10–15 mmHg. Interstitial oedema, characterised by peripheral septal (Kerley B) lines due to thickening of the interlobular septa, is thought to result in a PAWP greater than 20 mmHg, while alveolar oedema is present when PAWP exceeds 25 mmHg.52 However, this hierarchy of radiographic changes is not ubiquitous and may only be partially present, or indeed absent, even in cases of advanced HF.51
In the acute setting, when present in patients exhibiting the clinical features of HF outlined above, PVBD, interstitial oedema and alveolar oedema are all ‘high value’ signs; with specificities of up to 96 %, 97 % and 99 %, respectively (see Table 3).46,53–55 However, these signs are unsuitable as screening tools as sensitivity is poor for all three measures (see Table 3, respectively: PVDB 54 %, interstitial oedema 34 %, alveolar oedema 6 %) with a wide variability in prevalence.46,53–55 Increased cardiothoracic ratio was more common (prevalence 50–66 %) thus more sensitive but less specific (Table 3, 74 and 76 %, respectively).46,53–55 Nevertheless, the chest radiograph remains an imperfect tool for detecting cardiac enlargement, and a large observational series in the US demonstrated that up to 20 % of patients discharged with a diagnosis of AHF may have a completely ‘negative’ film with features of HF entirely absent.56,57 The above studies are all importantly limited by a lack of core laboratory analysis, and as such may reflect some diagnostic inaccuracy, although should certainly serve to caution physicians against excluding HF in symptomatic patients based on radiographic findings alone.