 Discussion Lung or Pulmonary Ultrasound: B-lines
Discussion Lung or Pulmonary Ultrasound: B-lines
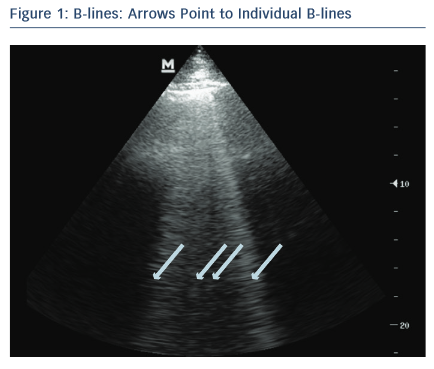
One of the most valuable and easiest to perform ultrasound assessments is lung ultrasound (LUS) looking for B-lines. LUS is performed using a low-frequency transducer – phased-array, microconvex or curvilinear probe – to allow for greater penetration and visualisation of B-lines.14,15 B-lines are vertical echogenic artifacts that originate from the pleural line, extend to the bottom of the ultrasound screen and move with lung sliding (see Figure 1).15,16 They are generated by water-thickened interlobular septa and may be seen in a variety of lung pathologies including pulmonary oedema.16–18 In the clinical setting of suspected AHF, pulmonary oedema is determined sonographically, using an eight-zone scanning technique, as greater than three B-lines in a rib space in at least two lung zones bilaterally.19,20 This finding on LUS is highly sensitive for the diagnosis of AHF, can be used to differentiate AHF from chronic obstructive pulmonary disease (COPD)14,16,18,21–24,10,25,26 and has better diagnostic accuracy for AHF than chest X-ray.15,27,28 In small studies, B-lines correlate well with natriuretic peptide levels8 and wedge pressure,28 though a more recent study shows only a modest correlation with filling pressures.29 In addition, LUS evaluation of B-lines is non-invasive, facile, feasible and has high inter-rater agreement.20,25 An alternative scanning protocol, counting the nu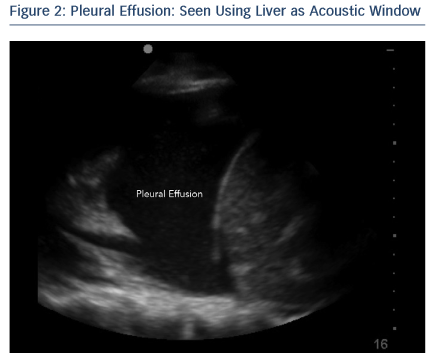 mber of B-lines in 28 total rib spaces bilaterally, may allow for a more precise quantification of pulmonary oedema.30,31 In AHF patients, B-line assessment aids in diagnosis and may guide acute management.13,17 Protocols that combine lung and cardiac ultrasound have been found to be highly accurate for diagnosing AHF13,32 and potentially more accurate than LUS alone.13
mber of B-lines in 28 total rib spaces bilaterally, may allow for a more precise quantification of pulmonary oedema.30,31 In AHF patients, B-line assessment aids in diagnosis and may guide acute management.13,17 Protocols that combine lung and cardiac ultrasound have been found to be highly accurate for diagnosing AHF13,32 and potentially more accurate than LUS alone.13
Pleural effusions
Pleural effusions are visualised sonographically as an anechoic or black fluid collection between the visceral and parietal pleura, in a dependent pattern (see Figure 2).15 Pleural effusions may be seen in AHF, as well as a variety of pulmonary pathologies including pneumonia and cancer.33 Literature is conflicting on whether the presence of a pleural effusion on LUS adds to the diagnosis of AHF. One study found pleural effusions were an unreliable finding in patients with AHF and less accurate than B-lines alone,25 while another study determined the presence of a pleural effusion combined with an ejection fraction <45 % to be highly specific for AHF and more accurate than B-line assessment alone.13