Cardiovascular Ultrasound: Inferior Vena Cava
Measurement of inferior vena cava (IVC) diameter, along with its variability with respiration to determine intravascular volume status, has been described for decades.34 IVC measurement and changes with respiration correlate with right atrial and central venous pressures.35–38 As use of has become more widespread, measurement of IVC to determine fluid responsiveness in multiple patient populations has become more commonplace.39,40 IVC size and collapsibility index should be measured in long axis caudal to the hepatic vein inlet, or in short axis at the level of the left renal vein (see Figure 3).41 In general, IVC size and collapsibility with respiration is most valuable at the extremes (volume overloaded – no collapse during inspiration, or volume depleted – positive inspiratory collapse) as a qualitative finding (see Figure 4). In a euvolemic patient, the IVC partially collapses during inspiration, reflecting negative intrathoracic pressure. Importantly, this applies only to patients breathing spontaneously. In mechanically ventilated patients, the opposite occurs during a respiratory cycle; during expiration, the negative intrathoracic pressure leads to partial collapse in a euvolemic patient. In patients who present with acute dyspnoea, a minimal change in IVC diameter with respiration may predict volume overload and helps to differentiate AHF from COPD.42,43
IVC measurement and changes with respiration correlate with right atrial and central venous pressures.35–38 As use of has become more widespread, measurement of IVC to determine fluid responsiveness in multiple patient populations has become more commonplace.39,40 IVC size and collapsibility index should be measured in long axis caudal to the hepatic vein inlet, or in short axis at the level of the left renal vein (see Figure 3).41 In general, IVC size and collapsibility with respiration is most valuable at the extremes (volume overloaded – no collapse during inspiration, or volume depleted – positive inspiratory collapse) as a qualitative finding (see Figure 4). In a euvolemic patient, the IVC partially collapses during inspiration, reflecting negative intrathoracic pressure. Importantly, this applies only to patients breathing spontaneously. In mechanically ventilated patients, the opposite occurs during a respiratory cycle; during expiration, the negative intrathoracic pressure leads to partial collapse in a euvolemic patient. In patients who present with acute dyspnoea, a minimal change in IVC diameter with respiration may predict volume overload and helps to differentiate AHF from COPD.42,43
Ejection Fraction (EF)
Ultrasound-trained emergency physicians can accurately determine left ventricular ejection fraction (LVEF) using both visual estimation and mitral E-point septal separation (EPSS) with good inter-rater reliability.44–46 Even with limited training, emergency physicians accurately estimate LVEF.47 However, EPSS is limited by septal wall motion abnormalities, mitral valve stenosis and angle of evaluation.48 Thus, the authors recommend EPSS be used in conjunction with other methods. If only a qualitative assessment of EF is desired, EPSS may be used to confirm visual estimation. International evidence-based recommendations advocate focused cardiac ultrasound be used to assess left ventricle dimensions and systolic function.6 Although a reduced EF in the setting of AHF signs and symptoms facilitates the diagnosis, the absence of a reduced EF does not rule it out. As nearly 50 % of patients with heart failure have a preserved EF, knowledge of the EF itself does not significantly alter acute management in the ER setting. The vast majority of AHF patients receive intravenous loop diuretics with a much smaller proportion receiving vasodilators. These treatments are given to AHF patients irrespective of EF and, at the present time, no robust evidence exists to suggest initial pharmacological management in the ER should differ based on EF.
Thus, ultrasound imaging of the heart may be more valuable to ‘rule-out’ other diagnoses rather than ‘ruling-in’ AHF. For example, presence of a significant pericardial effusion or right ventricular (RV) dilatation might suggest alternative diagnoses such as tamponade or pulmonary embolism.
Pitfalls
Ultrasound findings must be interpreted in clinical context. Although B-lines in the setting of a history and examination consistent with AHF most likely represent pulmonary congestion, B-lines lack specificity and are seen in multiple other conditions; for example, non-cardiogenic pulmonary oedema, pulmonary fibrosis, pneumonia, pneumonitis, and lung cancer.18,22,25 E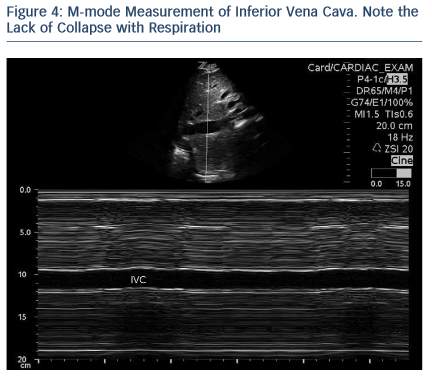 nsuring that B-lines are bilateral helps to differentiate AHF from other etiologies. Absence of B-lines in one hemi-thorax greatly lowers the probability of AHF.
nsuring that B-lines are bilateral helps to differentiate AHF from other etiologies. Absence of B-lines in one hemi-thorax greatly lowers the probability of AHF.
Some limitations in determining volume overload by measuring IVC diameter variability include etiologies that increase right atrial pressure outside of acute heart failure, such as pulmonary emboli, pulmonary hypertension, and cardiac tamponade. These examples highlight the importance of clinical context, as well as radiographic and biomarker features. In addition, these examples reveal the potential pitfall of examining the IVC only, rather than examining additional views of the lung and the heart.
As nearly half of heart failure patients have a relatively preserved EF, the condition is not excluded despite a normal EF.
While LUS is one of the easiest assessments to perform, IVC and LVEF evaluation may require some additional training; however, this is still well within the realm of many specialties.49,50 Importantly, focused cardiac ultrasound does not replace formal ECG;5 instead, focused bedside ultrasound aids in the diagnosis and management of many conditions, including AHF.