Future Directions
Multiple studies support the added value of a focused ultrasound to facilitate a diagnosis of AHF, but it remains infrequently used. As ultrasound devices become increasingly smaller and familiarity with focused ultrasound increases, its use will continue to grow. However, there are limited studies evaluating the utility of ultrasound to guide management and prognosis in the ER setting. Small studies have shown the efficacy of LUS to measure resolution of extra-vascular lung water or B-lines.17,51 Ongoing work in this area may demonstrate a future role for ultrasound to guide the management of AHF.
Conclusions
The ED plays a pivotal role in the initial management of AHF. Correct diagnosis and treatment is critical to ensure the right tone is set for subsequent in-hospi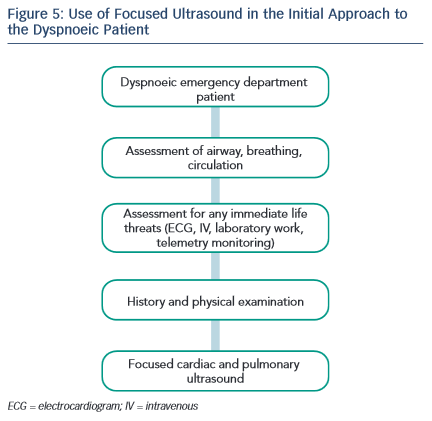 tal or outpatient management. As patients present with symptoms and signs and not diagnoses, AHF may be missed, especially in patients with other co-morbid conditions. Focused ultrasound is a fast, non-invasive method that rapidly aids the clinician to rule in or rule out various cardiac and pulmonary diagnoses. Importantly, focused ultrasound must be interpreted within the clinical context. For potential AHF patients, the use of LUS to assess for B-lines and pleural effusions, cardiac ultrasound to assess EF and measure IVC diameter and respiratory variation are skills that may be learned quickly and can aid the clinician.
tal or outpatient management. As patients present with symptoms and signs and not diagnoses, AHF may be missed, especially in patients with other co-morbid conditions. Focused ultrasound is a fast, non-invasive method that rapidly aids the clinician to rule in or rule out various cardiac and pulmonary diagnoses. Importantly, focused ultrasound must be interpreted within the clinical context. For potential AHF patients, the use of LUS to assess for B-lines and pleural effusions, cardiac ultrasound to assess EF and measure IVC diameter and respiratory variation are skills that may be learned quickly and can aid the clinician.
Clinical Case Study Conclusions
Given the patient’s history of coronary artery disease, AHF is on the differential diagnosis list – but so are acute coronary syndrome, COPD, and pneumonia. The ECG shows sinus tachycardia, but no other acute ischaemic changes. While awaiting chest X-ray, a focused ultrasound is performed, starting with the lungs (see Figure 5). Four or five B-lines are noted in at least two zones bilaterally, raising suspicion of pulmonary congestion. There are no pleural effusions. Cardiac examination does not show any pericardial effusion or RV dilation and systolic function appears mildly depressed by qualitative assessment. IVC assessment is difficult given the patient’s habitus, but minimal respiratory collapse is observed, suggesting elevated venous pressures. Based on this evidence, treatment is given for AHF. Chest X-ray reveals mild cardiomegaly, mild vascular engorgement, no Kerley B-lines, and no consolidation.