The STICH Trial
The STICH trial enrolled 1,212 patients with suitable coronary anatomy and an LVEF <35 % regardless of myocardial viability.12 Unfortunately, there was no genuine clinical equipoise between surgery and medical treatment. In those enthusiastic units that strongly advocated coronary artery surgery for heart failure, patients who were ‘good’ candidates for surgery including SVR received an operation and were not recruited into the trial. Moreover, as the trial progressed and recruitment became ever more difficult the entry criteria were subtly changed. This resulted in a trial not so much for heart failure as for ischaemia.
Nevertheless, the STICH trial is the only prospective, randomised controlled trial to specifically investigate the role of coronary artery surgery in patients with an LVEF <35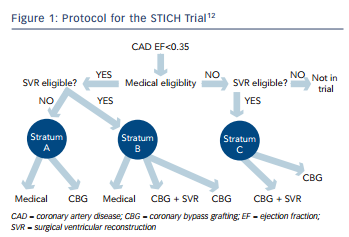 % who were also receiving guideline-directed medical treatment (for the trial protocol (see Figure 1). The trial tested two hypotheses among patients with an LVEF <35 % who were suitable for coronary artery bypass surgery. The surgical revascularisation hypothesis evaluated surgery compared with medical treatment alone (n=1,212) and the surgical ventricular reconstruction hypothesis compared surgery with and without SVR (n=1,000). Patients with Canadian Heart Association Functional Class lll or lV angina and those with left main stem stenosis >50 % were excluded from the surgical arm, but were eligible for the SVR arm. Medical treatment included renin–angiotensin–aldosterone system inhibitors, beta-blockers, statins and antiplatelet agents titrated to optimal doses; diuretic drugs and digoxin were also used. Where possible, surgical treatment included at least one pedicled internal mammary conduit; this was accomplished in 91 % of patients.12
% who were also receiving guideline-directed medical treatment (for the trial protocol (see Figure 1). The trial tested two hypotheses among patients with an LVEF <35 % who were suitable for coronary artery bypass surgery. The surgical revascularisation hypothesis evaluated surgery compared with medical treatment alone (n=1,212) and the surgical ventricular reconstruction hypothesis compared surgery with and without SVR (n=1,000). Patients with Canadian Heart Association Functional Class lll or lV angina and those with left main stem stenosis >50 % were excluded from the surgical arm, but were eligible for the SVR arm. Medical treatment included renin–angiotensin–aldosterone system inhibitors, beta-blockers, statins and antiplatelet agents titrated to optimal doses; diuretic drugs and digoxin were also used. Where possible, surgical treatment included at least one pedicled internal mammary conduit; this was accomplished in 91 % of patients.12
The Revascularisation Hypothesis
The 1,212 patients in the revascularisation hypothesis arm of the trial were enrolled in 99 sites in 22 countries.12 Using an intention-to- treat analysis, no significant difference was observed for the primary outcome of all-cause mortality between patients randomised to surgery versus medical treatment over a median follow-up period of 56 months. Of note, the surgery group had improved rates of death from cardiovascular causes and improved rates of a combined end- point of death from any cause plus admission to hospital for heart failure, which were pre-specified secondary outcomes.
Furthermore, Mark and colleagues showed that coronary artery surgery resulted in greater improvement in symptoms and quality of life than optimal medical treatment alone.17 Blinded end-point adjudication and mode of death analyses in the STICH trial revealed that surgery exerted a benefit across all common causes of death and death from myocardial infarction.18 These findings reveal an overall benefit of surgery against the background of modern medical treatment in patients with severe ischaemic left ventricular dysfunction.