STICH Subset Analysis
The initial target of this analysis was myocardial viability assessment, which was prospectively programmed into the design of the STICH trial.12 Multiple observation studies and meta-analyses had suggested that viability testing may be a powerful tool that will not only predict improvement in left ventricular function after coronary artery bypass surgery, but will identify patients with coronary artery disease and HFrEF with the greatest survival benefit from surgery compared with guideline-directed medical treatment.10,19 These studies were limited by their retrospective design, heterogenous methodology to define viability, lack of adjustment for key baseline variables (e.g. age and comorbidity) and the potential for selection of patients for surgery to have been influenced by the results of viability testing. Above all, these studies were performed before the modern era of medical treatment with few patients receiving beta-blockers.
In the original trial design, viability testing with single-photon emission computed tomography was required for entry to the study. But due to low recruitment, the protocol was revised to make single-photon emission computed tomography or viability testing with low-dose dobutamine echocardiography optional but strongly encouraged.20 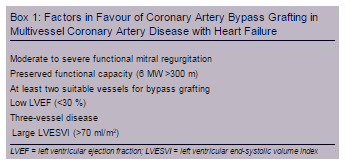 Thus only 601 of the 1,212 patients enrolled in the revascularisation hypothesis arm underwent assessment of myocardial viability. The viability analysis did not identify patients who would preferentially benefit from surgery. Unsurprisingly, over a median 5.1-year follow-up, patients with viable tissue had a lower mortality of 37 % versus 51 % in patients without myocardial viability. However, after adjustment for other prognostic variables, myocardial viability was not associated with improved survival suggesting that patient comorbidities and the severity of left ventricular remodelling are more important determinants of survival. Furthermore, there was no significant interaction with respect to mortality between viability status and assignment to surgery or medical treatment (p=0.53).
Thus only 601 of the 1,212 patients enrolled in the revascularisation hypothesis arm underwent assessment of myocardial viability. The viability analysis did not identify patients who would preferentially benefit from surgery. Unsurprisingly, over a median 5.1-year follow-up, patients with viable tissue had a lower mortality of 37 % versus 51 % in patients without myocardial viability. However, after adjustment for other prognostic variables, myocardial viability was not associated with improved survival suggesting that patient comorbidities and the severity of left ventricular remodelling are more important determinants of survival. Furthermore, there was no significant interaction with respect to mortality between viability status and assignment to surgery or medical treatment (p=0.53).
The lack of a significant interaction between viability and survival with surgical versus medical management of patients with severe ischaemic left ventricular dysfunction is reflected in the 2013 American College of Cardiology/American Heart Association Guidelines for the Management of Heart Failure.6 These guidelines indicate that in the absence of angina, coronary bypass surgery may be considered for improving survival in patients with ischaemic heart disease who have severe left ventricular dysfunction (LVEF <35 %) whether or not viable myocardium is present (class llb, level of evidence B). Although the primary viability assessment in the STICH trial was on the basis of a pre-determined dichotomous separation of patients with viable versus non-viable myocardium, a separate analysis in which the viability data were analysed as continuous variables also failed to show an association between myocardial viability and improved survival with surgery.21
Further analysis of imaging data in the STICH trial was performed to assess inducible myocardial ischaemia in 399 of 1,212 patients in whom stress imaging was performed using single-photon emission computed tomography or dobutamine echocardiography. This analysis failed to show enhanced survival with surgery in any subgroups.22 This was unexpected and ran counter to the prevailing wisdom from observational studies and previous trials in patients with normal left ventricular systolic function or less severe left ventricular dysfunction. Similarly, circulating levels of brain natriuretic peptide and soluble tissue necrosis factor alpha receptor-1 were strongly related to survival in both the surgical and medical cohorts, but did not identify those with a survival advantage with surgery.23
These data suggest that the observed survival benefits of coronary artery bypass surgery in patients with severe left ventricular dysfunction are driven primarily by factors other than biomarkers or objective markers of myocardial viability and ischaemia. Factors associated with higher survival rates with surgery include functional status as assessed by a 6-minute walk and the interaction of the angiographic severity of coronary artery disease, severity of left ventricular systolic dysfunction and severity of adverse left ventricular remodelling as assessed by end-systolic volume index. Patients with preserved effort tolerance but with multivessel disease, lower ejection fraction and higher left ventricular end-systolic volume index were most likely to benefit from surgery with respect to long-term survival (Box 1).