The Use of Home Blood Pressure Monitoring
Office BP measurement is associated with several disadvantages. Large variability in office BP readings have been reported, both in clinical trials5 and in the primary care setting.6 A study in which repeated BP measurements were made over a 2-week period under research study conditions found variations of as much as 30 mmHg with no treatment changes.7 A recent observational study required primary care physicians (PCPs) to measure BP on 10 volunteers. Two trained research ass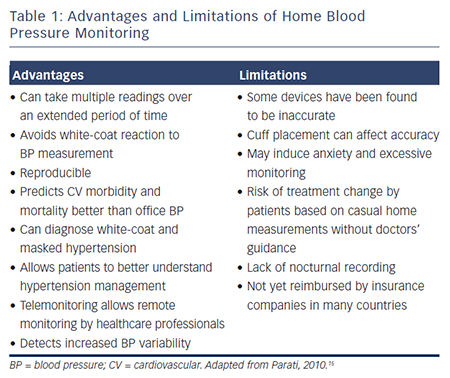 istants repeated the measures immediately after the PCPs. The PCPs were then randomised to receive detailed training documentation on standardised BP measurement (group 1) or information about high BP (group 2). The BP measurements were repeated a few weeks later and the PCPs’ measurements compared with the average value of four measurements by the research assistants (gold standard). At baseline, the mean BP differences between PCPs and the gold standard were 23.0 mmHg for systolic and 15.3 mmHg for diastolic BP. Following PCP training, the mean difference remained high (group 1: 22.3 mmHg and 14.4 mmHg; group 2: 25.3 mmHg and 17.0 mmHg). As a result of the inaccuracy of the BP measurement, 24–32 % of volunteers were misdiagnosed as having systolic hypertension and 15–21 % as having diastolic hypertension.6
istants repeated the measures immediately after the PCPs. The PCPs were then randomised to receive detailed training documentation on standardised BP measurement (group 1) or information about high BP (group 2). The BP measurements were repeated a few weeks later and the PCPs’ measurements compared with the average value of four measurements by the research assistants (gold standard). At baseline, the mean BP differences between PCPs and the gold standard were 23.0 mmHg for systolic and 15.3 mmHg for diastolic BP. Following PCP training, the mean difference remained high (group 1: 22.3 mmHg and 14.4 mmHg; group 2: 25.3 mmHg and 17.0 mmHg). As a result of the inaccuracy of the BP measurement, 24–32 % of volunteers were misdiagnosed as having systolic hypertension and 15–21 % as having diastolic hypertension.6
Two alternative technologies are available for measuring out-of-office BP. Ambulatory BP monitoring (ABPM) devices are worn by patients over a 24-hour period with multiple measurements and are considered the gold standard for BP measurement.8 The average of multiple measurements at home tends to be lower compared with the measurements in a surgery5 and is more reproducible than clinic measurements.5 It also has the advantage of measuring nocturnal BP and therefore allowing the detection of an attenuated dip during the night. However, ABPM monitors are expensive and, while cost-effective for the diagnosis of hypertension, are not practical for the long-term monitoring of BP.
In the past decade, HBPM has emerged as an effective and convenient means of screening for hypertension,4,9 as well as being costeffective.10 Methods for non-invasive BP measurement include auscultatory, oscillometric, tonometry and pulse wave record and analysis. HBPM uses the same technology as ABPM monitors, but allows patients to monitor BP as often as they wish. The advantages and disadvantages of HBPM are summarised in Table 1. While ABPM provides BP information at many timepoints on a particular day during unrestricted routine daily activities, HBPM provides BP information obtained under fixed times and conditions over a long period; thus, HBPM gives stable readings with high reproducibility and has been shown to be as reliable as ABPM.11–13
Recommendations for the Use of Home Blood Pressure Monitoring
National Institute for Clinical Excellence (NICE) guidelines14 for HBPM recommend that when using HBPM to confirm a diagnosis of hypertension it is necessary to ensure that:
Measurements taken on the first day should be discarded and the average value of the remaining days after day one is discarded be used.
Except for special cases (for example, patients with arrhythmias trained in auscultatory BP measurement), the use of auscultatory devices (mercury, aneroid or other) is not recommended for HBPM.15 Monitors that use the oscillometric method are accurate, reliable, easy to use and relatively inexpensive.16 Recommendations are in place to ensure the accuracy of monitoring devices:17–19 in the UK and Ireland the Dabl Educational Trust20 and the British Hypertension Society have produced lists of validated devices.21 The European Society of Hypertension Working Group on Blood Pressure Monitoring has produced a detailed consensus document on guidelines for HBPM.15 It recommends semiautomated (manual cuff inflation) or automated electronic devices that measure BP at the upper arm as the preferred option for HBPM. Such devices are easier to use and avoid observer bias. Monitors equipped with an automated memory should prevent patients from misreporting their BP measurements. Finger and wrist devices are less accurate and are not recommended, unless brachial measurements are difficult or impossible to obtain (for example, in subjects with very large arm circumference or extreme obesity).