Compliance and Improvement of Blood Pressure Control
Incorporation of HBPM into routine management of patients with uncontrolled hypertension may improve BP control. Several metaanalyses have shown that compared with usual care, the use of HBPM is associated with significant reductions in systolic and diastolic BP,48–51 as well as reductions in antihypertensive medication and therapeutic inertia, defined as unchanged medication despite elevated BP.50 While most studies have focused on white populations, some studies have looked at ethnically diverse adults with uncontrolled BP52,53 and highrisk patients (i.e. history of stroke, coronary heart disease, diabetes or chronic kidney disease (CKD) and with baseline BP of at least 130/80 mmHg) from clinics in low-income, medically underserved communities.54 Studies are also ongoing in stroke and at-risk groups.55
HBPM is most effective when accompanied by input from a healthcare professional, e.g. telemonitoring, whereby readings made at home are instantly relayed to a primary healthcare professional who can guide treatment along a predetermined algorithm in such a way that treatment is effected by readings obtained in a more direct manner.56–60 Numerous studies support the use of HBPM and telemonitoring,61–63 and other studies are planned.64 The use of telemonitoring avoids travel for the patient and saves time for the healthcare team. It has also been hypothesised that if patients can understand their own BP measurements an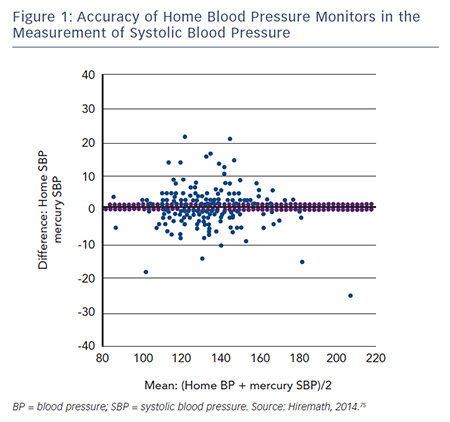 d appreciate the impact of treatment, then they may be more likely to comply with medical therapy in the longer term, even if the treatment does not appear to be making them feel better.4 There is a need for clinical trial data to confirm this hypothesis.
d appreciate the impact of treatment, then they may be more likely to comply with medical therapy in the longer term, even if the treatment does not appear to be making them feel better.4 There is a need for clinical trial data to confirm this hypothesis.
Some studies suggest that HBPM may contribute towards medication adherence in hypertensive patients,65,66 although others have not reached this conclusion.67 NICE guidelines still recommend ABPM where possible.
Cost-effectiveness of Home Blood Pressure Monitoring
A recent cost-benefit analysis found that HBPM is more effective than conventional clinic BP monitoring in the diagnosis and management of hypertension, is easier to implement and requires less labour and capital investment than ABPM.10,68
As a result of these findings, the American Heart Association, the American Society of Hypertension and the Preventive Cardiovascular Nurses’ Association have released a statement suggesting that HBPM be incorporated into usual care.16 European guidelines also support the use of HBPM as an adjunct to conventional office management.15,69
Limitations of Home Blood Pressure Monitoring
Patient Groups
Further research is required in the clinical application of HBPM in certain patient groups; this includes children and adolescents. A systematic review of 27 studies found that HBPM has similar diagnostic value in children as in adults and appears to be a reliable alternative to ABPM monitoring in the detection of white-coat hypertension. However, systolic daytime BP readings in children was found to be lower when measured with than daytime ABPM, whereas no such difference exists in adults.70 In patients with CKD, preliminary data suggest that HBPM outperforms office BP monitoring in predicting progression to end-stage renal disease or death.71 When combined with additional support such as telemonitoring, medication titration or behavioural therapy, HBPM results in a sustained improvement in BP control. However, HBPM does not provide nocturnal recordings and therefore cannot give information on diurnal patterns in BP, which are more prevalent in the CKD population and are important CV risk factors.71 Finally, caution should be exercised in the use of HBPM in the elderly. In a comparison of Korotkoff (K-BP, the traditional means of BP measurement employed in HBPM and office methods) and Strain-Gauge-Finger-Plethysmography (SG-BP) methods, K-BP underestimated BP in 46 % of subjects with SG-BP ≥140 mmHg at age 81.72
Accuracy of Home Blood Pressure Monitors
Accuracy of devices remains a limiting factor associated with HBPM. In a 2009 study to determine the accuracy of 554 automated HBPM devices, only 30 % of the devices were found to have acceptable validation, while 72 % of the automated monitors were inaccurate. The frequency of accuracy was higher among validated devices compared with non-validated devices.73 In a 2011 study, only 30 % of the 382 devices studied had been acceptably validated and 24 % of the devices were inaccurate. Upper arm devices were more accurate than wrist devices. The categorisation of upper arm devices into validated and ‘others’ showed that the validated devices were more accurate than the ‘others’.74 A recent retrospective review analysed ‘real use’ data from 210 patients attending hypertension clinics and found that 30 % of HBPM readings were >5 mmHg different and 8 % were >10 mmHg different from mercury systolic BP measurement taken in the clinic (see Figure 1). For diastolic BP, the proportions were 32 % and 9 %, respectively.75 In addition, a 2005 analysis of 30 studies found that the accuracy of most devices tends to decrease at higher BP levels.76 However, the study’s author suggested that the reported decrease in accuracy might be explained by the fact that BP is more variable at higher levels and by the use of sequential measurements.
The match between upper arm circumference and cuff size is essential to the accuracy of HBPM monitors; inappropriate cuff size has been associated with inaccuracy; studies have suggested that different cuffs should be used for BP measurement in child, adult and obese patients.77,78 The inflatable bladder of the cuff should cover 80–100 % of the individual’s arm circumference.15 The use of too small a cuff for the size of the arm can result in overestimation of BP, whereas a too large one results in an underestimation. Although standard cuffs are appropriate for most patients, in those with small (<24 cm) or large (>32 cm) arm circumference only the devices equipped with appropriate sized cuffs should be used.15 A study of six cuffs of various lengths and widths concluded a single long bladder cuff can measure BP with comparable accuracy both in subjects with large arms and in subjects with normal sized arms.79