Therapeutic Targets
As PO represents a medical emergency, treatment should be individually tailored to the urgency of the presentation, underlying pathophysiological mechanism, and acute haemodynamic characteristics. Clinical severity must be identified at the time of presentation, since the majority of the deaths occurred on the first day of admission.11 Systolic blood pressure (SBP) at presentation is one of the most cited predictors of in-hospital mortality in this subset of HF patients (see Table 2), and the recent guidelines recommend that patients with PO can be risk stratified even from the time of diagnosis and subjected to intense monitoring and treatments according to the value of SBP at admission.27 Beyond decongestion, rapid identification of precipitants and underlying aetiologies is a critical step in management of PO. As reported by 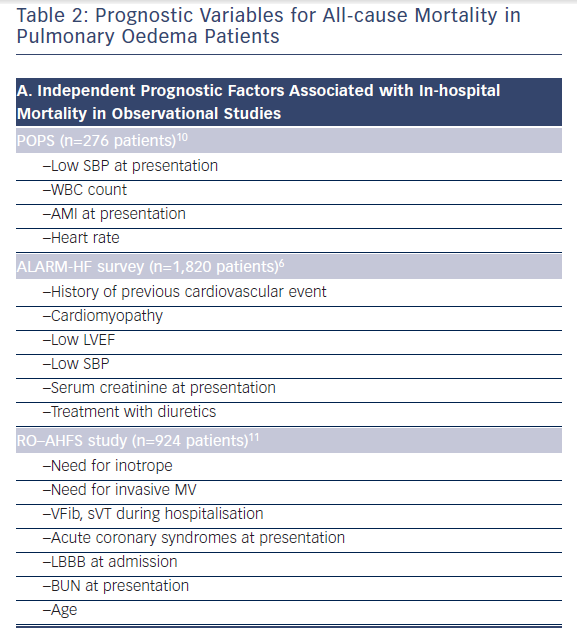
The immediate objectives of PO treatment are to improve symptoms, reestablish tissue oxygenation, and stabilize the patient’s haemodynamic condition. Rapid improvement of dyspnea constitutes a major treatment goal and offers an estimate of treatment efficacy. Although dyspnea is directly attributed to pulmonary congestion as result of acute increases in filling pressure, its mechanisms are multifactorial. Overall, imbalance between the neural output of the brain and the resulting work performed by the respiratory muscles may result in dyspnea.28,29 Sensation of dyspnea can be increased by vascular distension and interstitial oedema, which may directly stimulate pulmonary vascular nerve endings.30 Furthermore, an abrupt increase in pulmonary congestion directly leads to decreased pulmonary compliance, which further contributes to the tachypnea, tachycardia, and hypoxemia. Although, improved standardisation of dyspnea measurements has been proposed,31 a large area of uncertainty persists in terms of the factors associated with dyspnea relief.32 In spite of grading and scoring systems, in current clinical practice, evaluation of symptomatic improvement in the PO clinical profile is largely subjective and often based on clinician judgment.
The clinical picture of PO is dominated by pulmonary congestion along with acutely increased afterload. As relative volume redistribution plays a major role in the pathophysiology of the PO,13 the therapeutic strategies should focus on transitioning back into the venous reservoir. This aim can be achieved by:
An increase of left ventricular (LV) filling pressure and imbalances in Starling forces may explain transfer of fluids across alveolarcapillary membrane (see Figure 1). Further, the physiologic ability of alveolar epithelial cells to clear alveolar spaces from excess fluid is an active signalling process involving ion channels, mechanosensitive receptors, or adrenoreceptors.19,20,21,25 Very recent data suggest that targeting mechanisms that prevent barrier dysfunction26 and augment transepithelial sodium transport and enhance the clearance of alveolar oedema may lead to more effective prevention or treatment for PO.25,33
A search for the precipitant and underlying aetiology must be conducted early in the course of hospitalisation. It is important to identify those aetiologies that will not respond to conventional intravenous (IV) therapies, such as mechanical complications of AMI, valvular endocarditis, and prosthetic valve dysfunction. For these patients, mechanical circulatory support or rapid cardiac surgery may be life saving. Precipitant factors responsible for haemodynamic instability and the clinical presentation must also be identified and addressed.
Even if decreasing afterload is the main target for therapeutic intervention in PO patients, in some instances, hypoxemia may be too severe or may not be promptly improved by pharmacotherapies. Mechanical ventilation (MV), either invasive or noninvasive, when appropriately addressed, is an effective measure to correct hypoxemia by displacing fluid out of the alveoli. The need for MV, either invasive or noninvasive, must be anticipated in order to avoid waiting too long or in a place without the proper facilities. Noninvasive MV (NIMV) should be considered as adjunctive therapy in patients with PO who have severe respiratory distress and early initiation of NIMV may potentially correct metabolic abnormalities and reduce the proportion of patients requiring intubation.34
In particular circumstances, aggressive treatment of pulmonary congestion may alter the fine balance between end-diastolic pressure and end-diastolic volume, which will negatively impact cardiac output (CO), SBP, and end-organ perfusion (renal, coronary). As a result, some patients may experience worsening of ischemia, life-threatening arrhythmias, or a decline in renal function during hospitalisation. Consequently, in addition to decreasing pulmonary congestion, therapeutic strategies should prevent end-organ damage and not increase the risk for ischemia, propensity for cardiac arrhythmias, and/ or permanently alter intrarenal haemodynamics.