Technical Details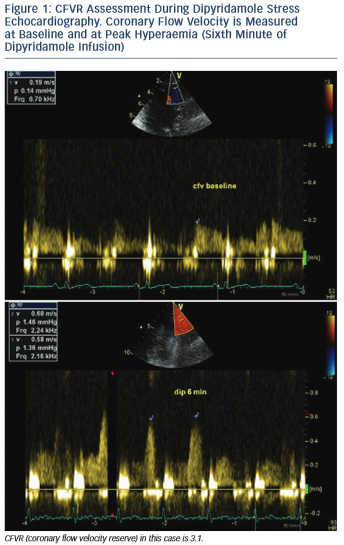
All three coronary arteries could be visualised with TDE and CFVR could be assessed. The left anterior descending (LAD) coronary artery has been the most commonly interrogated, followed by the posterior descending artery (PDA). Technical feasibility to investigate LAD is high with more than 90 % in experienced hands4–6 and reaches nearly 100 % with the use of intravenous contrast agents.7 The feasibility of CFVR assessment in PDA is lower – in the range between 54 and 86 %.4,5,8 Left circumflex coronary artery (LCx) is most challenging of the three due to the particular anatomy of the artery and the poor resolution of the lateral wall.2
Interobserver and intraobserver variability of CFVR measurements have been assessed in various studies and both are in the range of 5 %.9,10 Intra-individual variability has also been shown to be low.10
Settings
The appropriate setting of the echo scanner is an important prerequisite for CFVR assessment. LAD is visualised either with a high-frequency transducer (4–8 MHz) or with transthoracic low-frequency probe (3.5–5 MHz) with a second harmonic capability.2,11 PDA is situated more deeply in the chest and a low frequency transducer is needed to assess coronary flow.11,12 Color Doppler pulse repetition frequency should be 15–25 cm/s, wall filters set high and pulse Doppler filters should be low. Pulse wave Doppler sample volume should be 3–4 mm.2
Proximal or Distal to a Stenosis?
The best way to assess the functional significance of a stenosis is to evaluate the coronary flow in the distal tract of the artery according to the lesion. Proximal to the stenosis, CFVR could be normal because there are usually side branches bet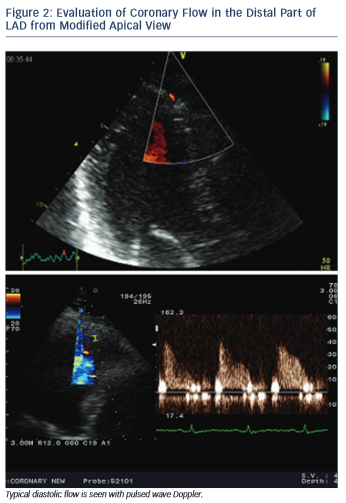 ween the sampling site and the stenosis with preserved perfusion in adjacent territories. At the site of the stenosis, the flow accelerates to compensate for lumen loss.2,14
ween the sampling site and the stenosis with preserved perfusion in adjacent territories. At the site of the stenosis, the flow accelerates to compensate for lumen loss.2,14
Considering the fact that CFVR is measured most commonly in the distal LAD and PDA, while the majority of relevant stenoses are located in the proximal to middle part of LAD and in the proximal right coronary artery (RCA) before the crux cordis, CFVR usually provides post-stenotic values.3
Echocardiographic Views
All three LAD segments (proximal, mid and distal) are visible with the new technical applications in TDE. CFVR is usually assessed in the distal and sometimes middle LAD segment. Distal LAD segment is evaluated from an apical view, somewhere between the classic two- and three-chamber view where the anterior interventricular groove runs, and near left-ventricular apex (see Figure 2). The mid- to-distal LAD segment is visualised in a modified left parasternal view with the patient in the left lateral decubitus position and the transducer moved lower and more lateral in order to visualise the anterior interventricular groove.15
PDA is assessed from a modified apical two-chamber view showing the posterior interventricular groove and adjacent to the ostium of the coronary sinus (see Figure 3).12 The distal LCx is searched at the basal and mid-portion of left ventricular lateral wall in an apical four- chamber view.13
When the appropriate position is achieved, the respective arte ry is searched for using color Doppler flow mapping and predominantly diastolic signal. Blood flow velocity is measured using pulsed wave Doppler echocardiography. Angle correction is not necessary since CFVR is a ratio between baseline and hyperaemic flow velocity and is not affected by the absolute value of flow velocity. Nevertheless, angle should be kept as low as possible (below 40°).2,15
ry is searched for using color Doppler flow mapping and predominantly diastolic signal. Blood flow velocity is measured using pulsed wave Doppler echocardiography. Angle correction is not necessary since CFVR is a ratio between baseline and hyperaemic flow velocity and is not affected by the absolute value of flow velocity. Nevertheless, angle should be kept as low as possible (below 40°).2,15
Systole or Diastole?
Coronary flow is biphasic with diastolic predominance. The blood supply to cardiac myocytes is largely diastolic due to the typical function of heart muscle – contracting in systole with generation of high intramural pressure, which impedes perfusion. Due to the translational motion of coronary arteries during the cardiac cycle it is sometimes difficult to obtain a complete Doppler signal throughout the cardiac cycle. This is not a problem, since only the diastolic flow is usually needed to assess baseline and hyperaemic coronary flow and calculate CFVR.2
Coronary flow velocities can be measured online or offline. Maximal flow velocity (averaging three cardiac cycles) at baseline and during hyperaemia is considered, although mean flow velocity could be used as well without influencing the final CFVR value, which represents the ratio between baseline and hyperaemic velocities. It should be emphasised that during administration of a vasodilating agent the probe must be kept in the same position and machine settings must not be changed compared with baseline.